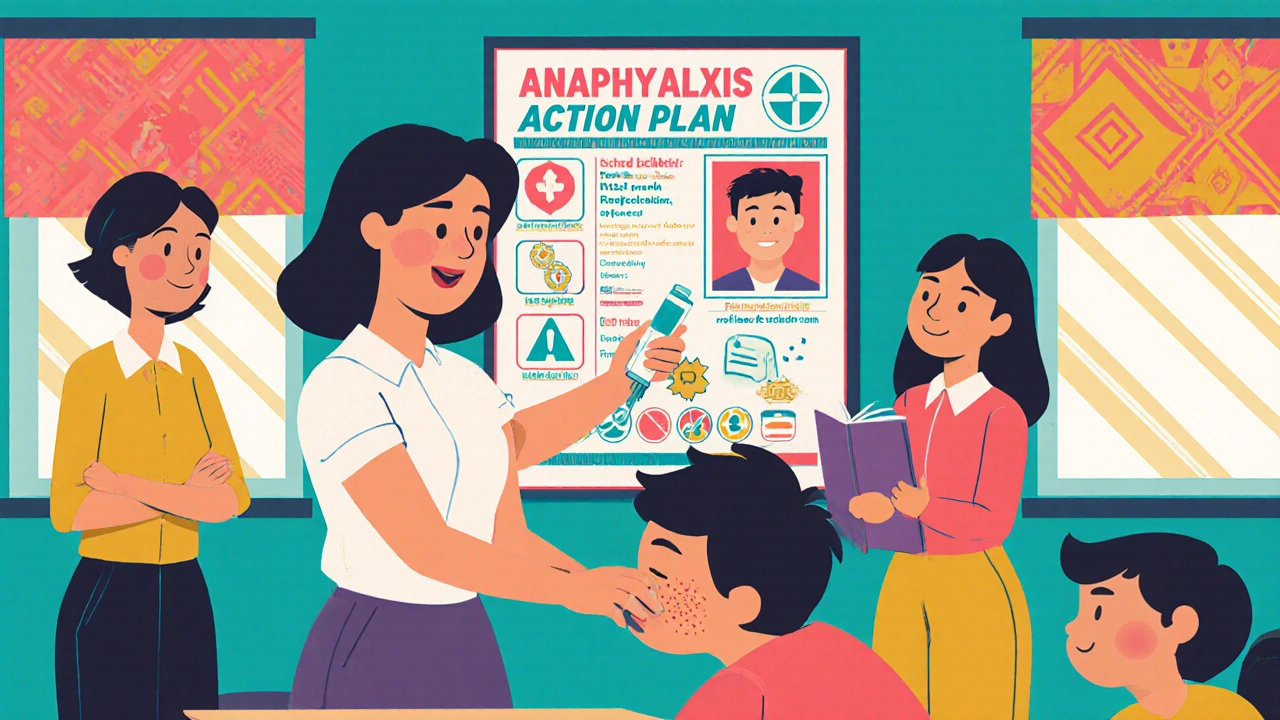
What an Anaphylaxis Action Plan Really Is
An anaphylaxis action plan isn’t just a piece of paper. It’s a life-saving roadmap. When someone has a severe allergy - to peanuts, shellfish, bee stings, or other triggers - their body can shut down in minutes. Without quick action, it can be fatal. This plan tells exactly what to do when that happens: who to call, where the medicine is, and how to use it. It’s not optional in schools or workplaces where people with serious allergies are present. It’s basic safety, like having a fire extinguisher in the hallway.
The CDC, FARE, and other major health groups agree: every person with a known risk of anaphylaxis needs a personalized plan signed by their doctor. It must include their photo, confirmed allergens, symptoms to watch for, and clear instructions to give epinephrine immediately. No waiting. No second-guessing. Epinephrine is the only thing that stops anaphylaxis from killing someone.
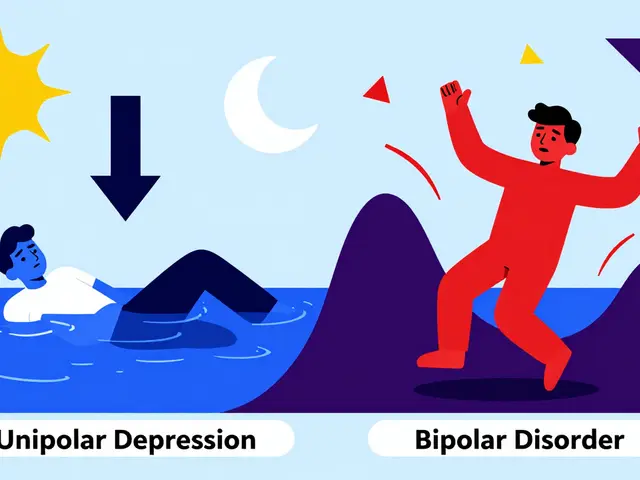
Why Epinephrine Is Non-Negotiable
Many people think antihistamines like Benadryl are the first response to an allergic reaction. They’re not. Antihistamines might help with a rash or itchy nose, but they do nothing to stop the body from going into shock. Only epinephrine can reverse the swelling in the airway, raise dropping blood pressure, and prevent cardiac arrest.
Studies show that if epinephrine isn’t given within five minutes of symptoms starting, the chance of death or serious injury jumps by 68%. A 2020 study in the American Family Physician journal found that delays in epinephrine use increased mortality risk by 83%. That’s not a small risk. That’s a preventable tragedy.
That’s why every action plan must say this in plain language: Give epinephrine first. No exceptions. If two or more body systems are reacting - like hives and vomiting, or swelling and trouble breathing - epinephrine goes in. Right now. No one should be afraid to use it. No one should wait for permission.
What’s in a School’s Anaphylaxis Action Plan?
Schools have the most structured system in place. As of 2024, 49 U.S. states have laws requiring schools to have epinephrine available and staff trained to use it. The CDC’s 2024 guidelines say every student with a known allergy needs an individualized plan, signed by their doctor, kept on file, and reviewed every year.
Here’s what a good school plan includes:
- A photo of the student for quick identification
- Confirmed allergens (e.g., “peanuts, tree nuts, milk” - not just “food allergies”)
- Clear symptom list: mild (itching, hives) vs. severe (wheezing, dizziness, loss of consciousness)
- Step-by-step instructions: “Administer epinephrine immediately if breathing is affected”
- Emergency contacts (parents, backup caregivers)
- Location of epinephrine - unlocked, visible, and within 60 seconds of every classroom
And it’s not just for the allergic student. Schools must train at least two staff members per classroom to use epinephrine auto-injectors. That means teachers, aides, cafeteria workers, bus drivers - anyone who might be with the child during the day. Annual training is required, not optional. Yet, only 37% of schools actually do it every year, according to the National Association of School Nurses.

Workplace Plans Are Lagging - and People Are Dying Because of It
While schools have clear rules, workplaces are a mess. Only 28 states have specific laws about anaphylaxis in the workplace. Most employers don’t have a plan unless they’re forced to by law or a lawsuit.
Under the Americans with Disabilities Act, employers must make reasonable accommodations for employees with severe allergies. That includes letting them carry their own epinephrine, storing it in an accessible place, and training staff to respond. But in practice? It rarely happens.
A 2022 FARE survey found that 57% of employees with severe allergies had at least one reaction at work where no one helped. Why? Fear. Confusion. Lack of training. One server with a shellfish allergy told Reddit: “My manager said keeping my epinephrine unlocked behind the counter was against policy. I had to run to the bathroom and inject myself alone.”
Employers think they’re protected by not having a plan. They’re wrong. If someone dies because no one knew how to respond, the company can be sued for negligence. OSHA requires first aid to be available - and anaphylaxis is a medical emergency. Not having a plan isn’t just careless. It’s legally risky.
How to Build a Real Action Plan - Not Just a Form
Having a plan on paper doesn’t mean anything if no one knows how to use it. The best plans are simple, visual, and practiced.
Start with FARE’s or AAFA’s official template - they’re free, updated yearly, and used in 78% of U.S. school districts. Don’t use a generic form from your district unless it’s been reviewed by an allergist. Most school forms are too vague. One educator told FARE: “Our form said ‘watch for symptoms.’ That’s not enough.”
Here’s how to make it work:
- Get the doctor’s signature - and make sure they write the exact allergens. “Dairy” is fine. “Milk products” is not.
- Put the plan in every location where the person spends time: classroom, cafeteria, bus, desk, break room.
- Store epinephrine where it’s instantly accessible - not locked in a cabinet, not in a drawer, not in the nurse’s office unless it’s right next door.
- Train everyone who might be nearby. Not just “the nurse.” Everyone. Use video training. Practice on trainers. Test them.
- Review the plan every year. Allergies change. Contacts change. People leave. Plans get outdated.
And here’s the hard truth: if you’re the one with the allergy, you can’t rely on others. Always carry two epinephrine pens. Never let them expire. Tell people - clearly - what to do if you collapse. Don’t assume they’ll know.

What Happens When the Plan Works - And When It Doesn’t
When it works, it’s quiet. No drama. No panic. A teacher sees a child rub their eyes and start coughing after eating a snack. They check the plan. They grab the epinephrine. They give the shot. They call 911. Within 90 seconds, the child is being helped. No long-term damage. No hospital stay. Just relief.
That’s what happened to Sarah Johnson’s daughter. Her school used FARE’s plan. Staff were trained. When the reaction hit, the teacher acted immediately. Her daughter was fine.
But when it doesn’t work? It’s devastating. A child dies because the epinephrine was locked up. An adult collapses at work and no one knows what the pen is for. A manager says, “I don’t want to be sued if I use it.” That’s not a policy. That’s a death sentence.
The CDC warns against “watch and wait.” If you’re unsure, give epinephrine. It’s safe. Even if the person doesn’t need it, the side effects are minor - a racing heart, some shakiness. Not giving it? That’s the risk that kills.
What’s Changing in 2025 - And What You Should Do Now
The field is moving fast. In March 2024, FARE launched a digital action plan platform that lets families update allergens and contacts in real time. Schools using it report 40% fewer errors in plan details. The CDC added new guidelines for field trips and after-school activities - because reactions don’t happen only during class hours.
By 2025, the FDA may approve new epinephrine pens with voice prompts. Imagine a device that says, “Press here. Hold for 3 seconds.” That could help workplaces where no one has been trained. But waiting for tech isn’t an option. Right now, the tools exist. The knowledge exists. What’s missing is action.
If you’re a parent: demand the official plan. Ask for training records. Know where the pens are stored. Don’t accept vague answers.
If you’re a teacher or employer: get the FARE template. Train your team. Store epinephrine where it’s visible and reachable. Make it part of your safety culture - like CPR or fire drills.
If you live with a severe allergy: carry two pens. Tell people. Don’t be afraid to speak up. Your life depends on it.
What to Do If You’re Not Sure
Still not sure where to start? Here’s the simplest checklist:
- Does the person have a doctor-signed plan with a photo?
- Are two epinephrine pens always accessible and not expired?
- Have at least two people been trained to use them?
- Is the plan reviewed every year?
- Is everyone aware of the allergens and symptoms?
If you answered “no” to any of these - fix it now. Not tomorrow. Not next month. Now. Because when anaphylaxis strikes, there’s no time to learn.

November 25, 2025 AT 01:00 AM
I work in a school and we just got new epinephrine kits last month. 🙌 No more locked cabinets-now they’re in every classroom, by the gym, even on the bus. My 3rd grader has a peanut allergy and I cried when I saw the teacher practice with the trainer pen. This isn’t just policy-it’s love in action.
November 26, 2025 AT 22:02 PM
man i just found out my cousin’s kid had a near miss at daycare last year because the nurse was on lunch and no one knew where the epi pen was. we’re talking 2 minutes before someone called 911. that’s too long. why is this still not mandatory everywhere? like... come on.
November 27, 2025 AT 21:56 PM
THEY’RE LYING TO YOU. EPINEPHRINE ISN’T SAFE. IT’S A BIG PHARMA TRICK TO MAKE YOU DEPENDENT. THEY WANT YOU TO THINK YOU NEED IT EVERY TIME YOU EAT PEANUT BUTTER. THE REAL TRUTH? YOUR BODY CAN HEAL ITSELF IF YOU JUST STOP FEARING FOOD. THEY CONTROL THE NURSES. THEY CONTROL THE SCHOOL DISTRICTS. THEY CONTROL YOUR MIND.
November 29, 2025 AT 00:10 AM
look i get it, epinephrine saves lives, but let’s be real-how many people actually know what anaphylaxis looks like? i’ve seen people panic over a little red spot on their arm and call 911. meanwhile, the guy who’s turning blue from swelling gets ignored because everyone’s too busy Googling ‘is this hives or just a rash?’ we need to stop treating allergies like a movie plot and start treating them like the medical emergency they are. training isn’t optional. it’s survival 101.
November 30, 2025 AT 17:58 PM
I’ve read the CDC guidelines. I’ve reviewed FARE’s templates. And I’ve personally trained 17 staff members in my district. If your school doesn’t have a signed, photo-included, allergen-specific plan with two accessible epinephrine auto-injectors and annual training logs-you are not just negligent. You are a danger. And yes, I will be reporting you.
December 2, 2025 AT 16:12 PM
The institutionalization of epinephrine protocols represents a paradigmatic shift in public health policy, wherein the bioethical imperative of preemptive intervention supersedes traditional notions of individual autonomy. One must consider the ontological weight of the epinephrine auto-injector as not merely a pharmacological device, but as a semiotic artifact of societal responsibility.
December 4, 2025 AT 04:00 AM
I’m from India and we don’t have this kind of system here. My sister had a reaction at work last year and no one knew what an EpiPen was. They gave her antihistamines. She almost died. I’m sharing this with my HR department tomorrow. This post is a wake-up call.
December 4, 2025 AT 19:38 PM
if you have a kid with allergies you need to do 3 things: 1. get the doctor to sign the plan 2. make sure there are two pens at school and they’re not expired 3. tell every teacher coach bus driver babysitter what to do. don’t assume they know. don’t hope they’ll figure it out. say it loud. say it clear. your kid’s life depends on you being the annoying parent
December 6, 2025 AT 05:46 AM
in my country we don’t have laws like this but i’ve been pushing my workplace to adopt this since my colleague had a reaction last year. we now have epinephrine in the kitchen, training videos on our intranet, and even a poster with symptoms on the wall. it took 8 months but now people actually know what to do. it’s not hard. it’s just about caring enough to do it. if you’re reading this and you’re an employer-stop waiting for someone to die before you act.
December 7, 2025 AT 05:36 AM
I’m sorry, but if your child has a peanut allergy, and you’re sending them to a school that doesn’t have a 100% peanut-free zone, you’re not being a good parent. Epinephrine is a band-aid solution. The real solution is eliminating the allergen entirely. You’re putting other children at risk by allowing peanuts anywhere near them. This isn’t about accommodation-it’s about responsibility.
December 7, 2025 AT 19:35 PM
so like... i get that epinephrine saves lives but honestly? most of these plans are just for show. everyone’s too scared to use them. i’ve seen teachers freeze when someone sneezes near a nut. it’s not about the plan-it’s about people being useless. also, why do we even have to do this? why can’t people just not bring nuts to school? simple.
December 8, 2025 AT 20:25 PM
they’re coming for your epinephrine next. first it’s peanut butter, then it’s dairy, then it’s gluten, then it’s AIR. they’re turning schools into sterile labs. the government’s using allergies to control behavior. you think they want you to live? no. they want you to obey. the epi pen is a tool of compliance. the real danger isn’t the allergy-it’s the system that profits from your fear.
December 10, 2025 AT 19:34 PM
i just want to say that i’ve been living with a shellfish allergy for 18 years and i’ve had 7 reactions. every single time, someone asked if i was 'just being dramatic.' i’m not dramatic. i’m dying. and now i’m supposed to trust strangers with my life? no. i carry two pens. i tell everyone. i don’t wait for a plan. i make my own. and if you think this is about 'accommodation'-you don’t get it.
December 12, 2025 AT 15:01 PM
i’ve been thinking about this all day. it’s not about the pens. it’s about the silence. the silence when someone’s face swells and no one moves. the silence when the manager says 'we don’t have time for this.' the silence when the parent whispers 'they didn’t know what to do.' we don’t need more laws. we need people who aren’t afraid to act. we need courage. not policy.
December 14, 2025 AT 13:53 PM
While the intention behind institutionalizing anaphylaxis protocols is laudable, one must interrogate the epistemological foundations of such measures. Are we, as a society, reducing complex physiological phenomena to binary response protocols? Is the auto-injector becoming a fetishized object of security, obscuring the deeper social determinants of allergic prevalence? The commodification of emergency care, while pragmatically expedient, risks infantilizing the patient and depersonalizing the medical encounter.
December 15, 2025 AT 00:31 AM
Oh, so now we’re supposed to train EVERYONE? Because clearly, the only reason people don’t know what to do is because they haven’t been told. Not because they’re lazy. Not because they don’t care. Not because they’re terrified of accidentally killing someone with a needle. No. It’s just lack of a PowerPoint. 🙄