Most people drink coffee without thinking twice. But if you’re on medication, that morning cup could be doing more than just waking you up-it might be making your pills less effective, or even dangerous. Caffeine isn’t just a harmless stimulant. It’s a powerful chemical that interferes with how your body processes many common drugs. And the risks aren’t theoretical. Real people are ending up in emergency rooms because they didn’t know coffee and their blood thinner don’t mix.
How Caffeine Messes With Your Medications
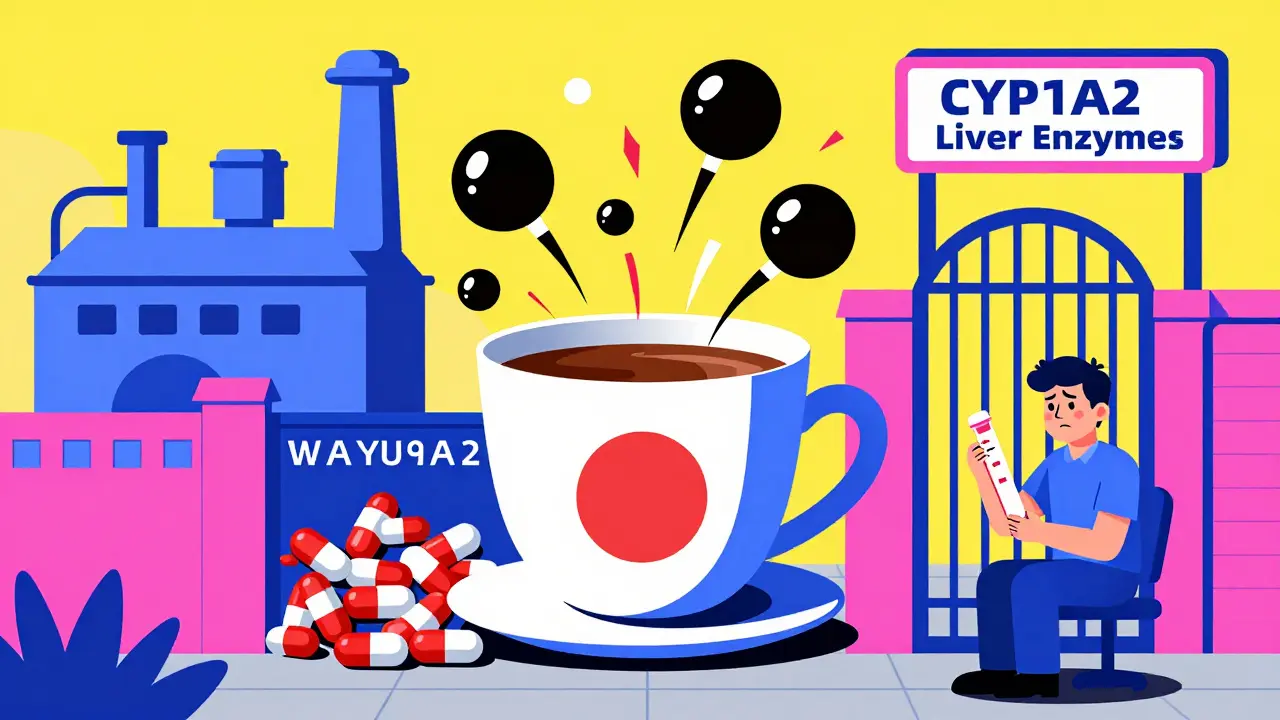
Caffeine doesn’t just buzz through your system like sugar. It actively blocks enzymes in your liver-especially CYP1A2-that are responsible for breaking down over 10% of all prescription drugs. When caffeine sits in your system, it slows down how fast your body clears out medications. That means those drugs stick around longer, building up to unsafe levels. Or sometimes, caffeine blocks absorption in your gut, so your pill never even gets into your bloodstream.
Think of it like a traffic jam at a drug processing plant. Caffeine is the truck that parks right in front of the gate. Other drugs-like warfarin, levothyroxine, or theophylline-can’t get through. The result? Either too much drug in your blood (risking overdose) or too little (making treatment useless).
High-Risk Medications: The Big Three
Not all drugs react the same way. Some are barely affected. Others? They’re ticking time bombs when paired with caffeine.
1. Blood Thinners (Warfarin and Others)
Warfarin is one of the most common medications linked to caffeine interactions. When you drink coffee, caffeine inhibits the enzyme that breaks down warfarin. That causes your INR-a measure of how long your blood takes to clot-to spike by 15-25% within 24 hours. An INR above 4.0 is dangerous. It means you’re at serious risk of bleeding inside your brain, stomach, or elsewhere.
A University of Michigan survey found that 41% of warfarin patients who drank more than 200 mg of caffeine daily (about two strong coffees) had unexplained INR spikes above 4.0. Nearly 1 in 6 of them ended up in the ER with bleeding. The FDA now requires warning labels on warfarin packaging: “Maintain consistent caffeine intake. Avoid sudden increases.” One coffee a day? Fine. Switching from one to four? That’s a medical emergency waiting to happen.
2. Thyroid Medication (Levothyroxine)
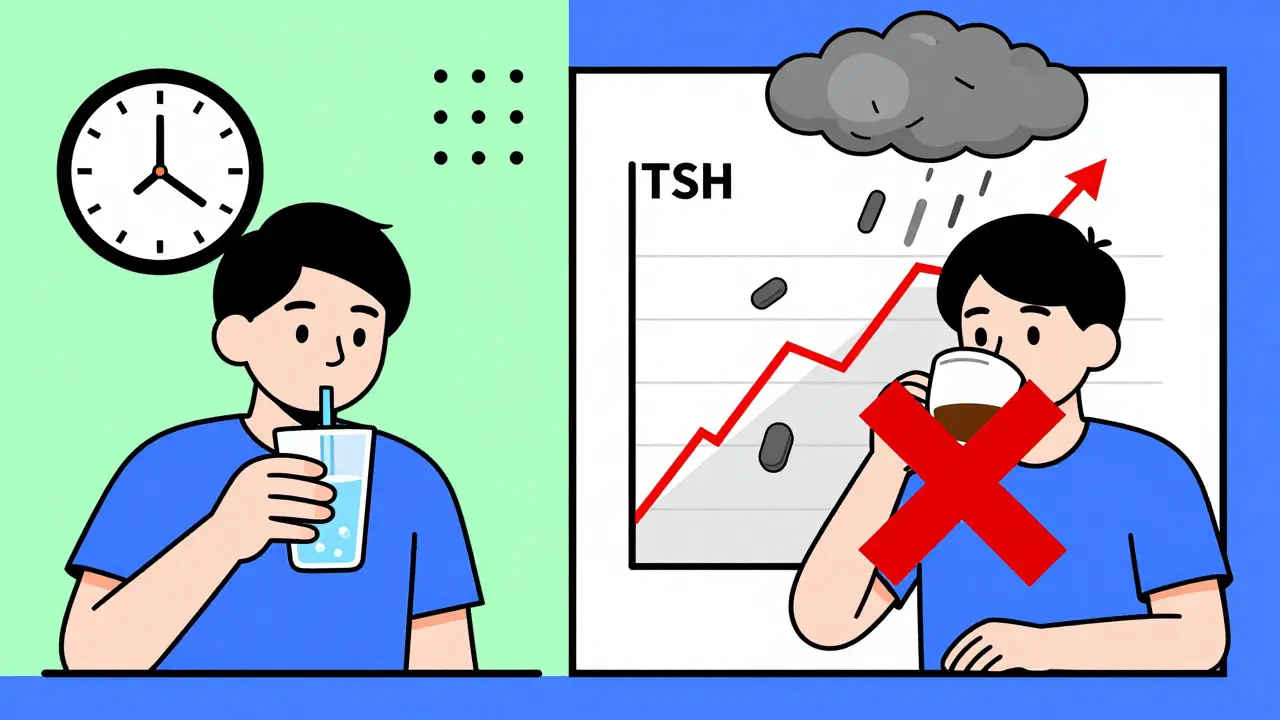
If you take levothyroxine for hypothyroidism, drinking coffee with your pill can cut its absorption by up to 55%. That’s not a small drop. It’s enough to throw your entire hormone balance off.
One Reddit user, ‘ThyroidWarrior2023,’ shared that after taking levothyroxine with coffee for three weeks, their TSH level jumped from 1.8 to 8.7-well above the normal range. Their endocrinologist confirmed: coffee was the culprit. The American Thyroid Association now recommends waiting at least 60 minutes after taking levothyroxine before drinking coffee. Some doctors suggest taking it first thing in the morning with water, then waiting until after breakfast to have your coffee.
3. Asthma Medications (Theophylline)
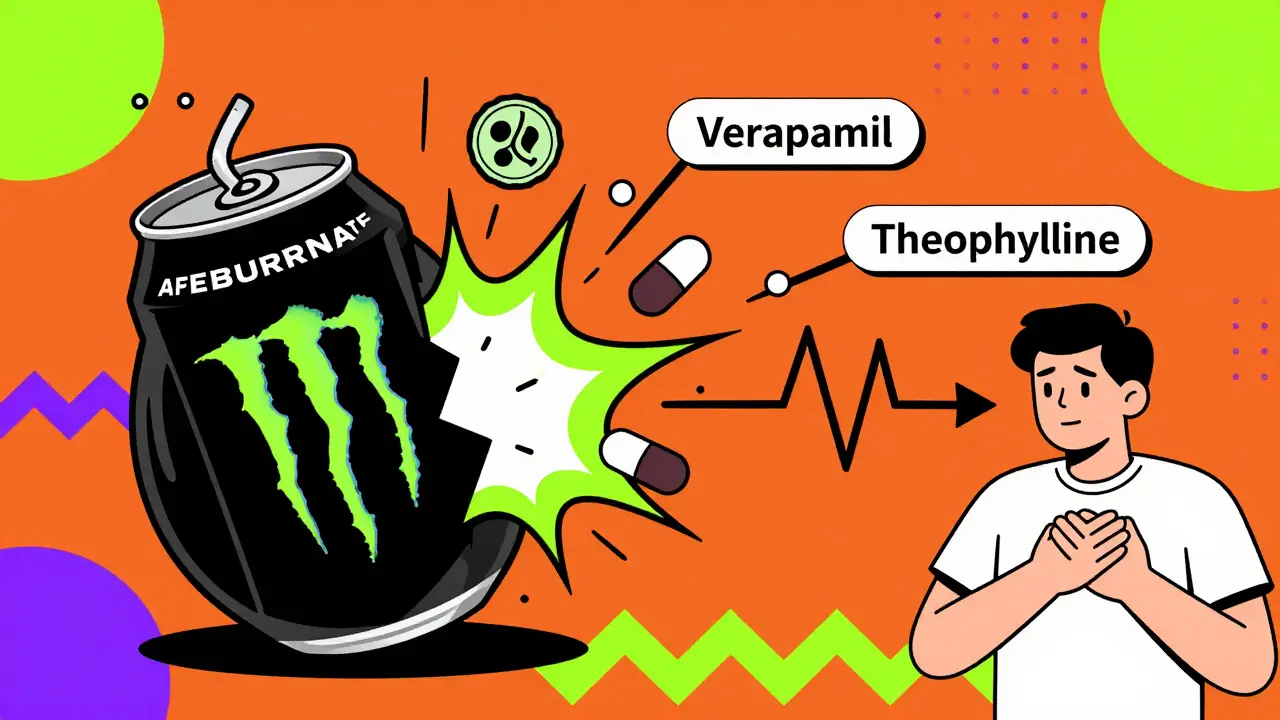
Theophylline and caffeine are chemically almost identical. They both use the same liver enzyme (CYP1A2) to get processed. When you take theophylline and drink coffee, your body can’t tell them apart. The result? Caffeine piles on top of theophylline, pushing blood levels up by 15-20%. That’s enough to trigger nausea, rapid heartbeat, tremors, or even seizures-even if you’re taking the correct dose.
University Hospitals’ 2025 guidelines advise asthma patients on theophylline to limit caffeine to under 100 mg per day (one small coffee). They also recommend monitoring heart rate: if it climbs above 100 bpm, it’s a red flag.
Other Dangerous Pairings
It’s not just the big three. Many other common drugs have hidden risks.
- Antidepressants (SSRIs): Fluvoxamine, in particular, interacts badly with caffeine. Harvard Health found caffeine reduces SSRI absorption by about 33%. That means your depression meds stop working as well. Users report increased anxiety, jitteriness, and mood swings.
- Heart Medications (Verapamil): Verapamil lowers blood pressure. Coffee can reduce its effect by 25-30%. Dr. David Musnick from Harvard explains this is due to caffeine blocking absorption in the intestines. The fix? Take coffee at least two hours before or after your pill.
- Stress Test Drugs (Adenosine, Dipyridamole): If you’re scheduled for a cardiac stress test, you must avoid caffeine for 24 hours. Even one cup of coffee can make the test useless-reducing its accuracy by 70-90%. Hospitals now send patients written instructions: “No coffee, tea, soda, or chocolate for 24 hours before your test.”
- Cold and Allergy Meds (Pseudoephedrine): Pseudoephedrine already raises heart rate and blood pressure. Add caffeine? That combo can spike your heart rate by 20-30 beats per minute. Dr. John Higgins at UT Southwestern calls it a “one-two punch.”
- Ephedrine: This stimulant, found in some weight-loss and decongestant products, becomes deadly when mixed with caffeine. Mayo Clinic data shows a 47% higher risk of hypertensive crisis, with systolic blood pressure rising over 30 mmHg in nearly 7 out of 10 cases.
Energy Drinks Are Worse Than Coffee
Many people think switching from coffee to energy drinks is healthier. It’s not. Energy drinks pack 80-300 mg of caffeine per can-sometimes more than a whole pot of coffee. But they don’t stop there. They also contain taurine, ginseng, guarana, and sugar. These ingredients don’t just add flavor-they interfere with drug metabolism too.
A 2021 study in PMC8541613 found energy drinks posed higher interaction risks than coffee alone. The FDA reported a 37% increase in caffeine-medication adverse events between 2020 and 2024, with 68% of serious cases linked to energy drinks. One 20-year-old in Ohio ended up in the ICU after mixing an energy drink with his antidepressant and blood pressure pill. His heart rate hit 180 bpm. He survived. Others haven’t.
What You Should Do
You don’t have to quit coffee. But you need to be smart.
- Know your meds. Check the label. If it says “avoid caffeine” or “may interact with stimulants,” pay attention.
- Time it right. For thyroid meds: wait 60 minutes after taking your pill. For blood pressure meds: wait two hours. For warfarin: keep your caffeine intake consistent. Don’t switch from one cup to five.
- Track your intake. A cup of brewed coffee has 95-200 mg caffeine. Tea: 20-60 mg. Soda: 30-40 mg. Energy drinks: 80-300 mg. Keep a simple log. Write down what you drink and when.
- Ask your pharmacist. Pharmacists are trained to catch these interactions. They see your full med list. Ask: “Does caffeine interfere with any of these?” Don’t assume they’ll bring it up.
- Watch for symptoms. Unexplained anxiety, rapid heartbeat, dizziness, or worsening symptoms on your meds? It might not be your disease-it might be your coffee.
Why So Many People Don’t Know This
A JAMA Internal Medicine study in April 2024 found that 62% of patients had no idea caffeine could interfere with their medications-even though 89% drank it daily. Doctors don’t always bring it up. Labels aren’t always clear. And caffeine feels harmless because it’s everywhere.
The American Pharmacists Association responded by making caffeine interaction screening mandatory in their 2023 certification update. Pharmacists now have to check for 17 high-risk combinations during medication reviews. That’s progress. But it’s not enough. Patients need to be the first line of defense.
The Future: Personalized Advice
Scientists are now studying why some people are more sensitive than others. It’s not just how much coffee you drink-it’s your genes. The CYP1A2 enzyme works differently depending on your DNA. Some people break down caffeine in an hour. Others take nine. That’s why two people can drink the same coffee, take the same pill, and have completely different outcomes.
The NIH launched a $4.7 million study in January 2025 to map how genetic differences affect caffeine-warfarin interactions. Epic Systems, one of the largest electronic health record providers, rolled out a pilot program in 47 hospitals in April 2025. It flags patients on high-risk meds and warns them about caffeine. Early results? A 29% drop in interaction-related ER visits.
By 2028, experts predict personalized caffeine guidance-based on genetic testing-will become standard. Until then, treat caffeine like any other drug. It’s powerful. It’s unpredictable. And if you’re on medication, it’s not worth the risk.
Can I drink coffee if I’m on warfarin?
You can, but you must be consistent. Drinking one cup of coffee daily is usually fine. But if you suddenly switch to three or four cups, your INR can spike dangerously. The FDA advises keeping caffeine intake steady. Don’t increase it by more than 100 mg per day. If your INR becomes unstable, cut caffeine for a week and retest.
Does decaf coffee have caffeine?
Yes. Decaf coffee still contains 2-15 mg of caffeine per cup. For most people, that’s not a problem. But if you’re on theophylline, warfarin, or a sensitive medication, even small amounts can add up. If you’re trying to eliminate caffeine entirely, switch to herbal tea or water.
Can I take my pill with tea instead of coffee?
Black tea has less caffeine than coffee, but it still has 20-60 mg per cup. Green tea has even less, but it’s not caffeine-free. If you’re on levothyroxine or warfarin, tea can still interfere. The safest approach is to take your pill with plain water and wait at least 60 minutes before drinking any caffeinated beverage.
I take antidepressants. Should I stop drinking coffee?
Not necessarily-but be cautious. Fluvoxamine, in particular, interacts strongly with caffeine, reducing its effectiveness and increasing anxiety. If you notice your mood worsening, or you feel jittery and anxious after coffee, try cutting back. Switch to half-caf or limit yourself to one small cup in the morning. Talk to your doctor if symptoms persist.
What if I accidentally drank coffee with my thyroid pill?
One mistake won’t ruin your treatment. But if it happens regularly, your thyroid levels will drift out of range. Don’t panic. Skip your next coffee. Take your pill with water tomorrow morning, and wait 60 minutes before drinking anything else. Schedule a TSH blood test in 6 weeks to make sure your levels are back on track.


December 22, 2025 AT 04:13 AM
ok so i just took my thyroxine with my morning coffee and now im panicking like its 2003 and i forgot my homework
December 24, 2025 AT 00:29 AM
man i used to chug espresso before my blood pressure meds and never thought twice. now i feel like i’ve been playing russian roulette with my arteries.
December 24, 2025 AT 21:05 PM
the real tragedy isn’t the caffeine-it’s that we’ve been trained to treat our bodies like disposable machines. you wouldn’t pour gasoline into a Tesla and expect it to run smooth, but we do this with our biology every damn day. coffee isn’t the villain. ignorance is.
December 26, 2025 AT 12:05 PM
it’s fascinating how something so culturally embedded-coffee, the daily ritual, the social lubricant-can be a silent saboteur of pharmacology. we treat it like water, but it’s more like a molecular key that jams the lock of our metabolic machinery. we don’t see the gears grinding until the machine breaks.
December 26, 2025 AT 16:01 PM
american healthcare is a joke. they sell you coffee then act shocked when you die from it. in india we just drink chai with our pills and live longer. maybe we dont need all this science
December 28, 2025 AT 01:42 AM
as a pharmacist, i see this every day. patients will tell me they take warfarin and drink 3 lattes a day, then wonder why their INR is 6.5. the problem isn’t the drug-it’s the lack of communication. pharmacists aren’t mind readers. if you don’t tell us you’re drinking 12 oz of espresso before breakfast, we can’t help you.
the FDA warning is there for a reason. consistency isn’t just a buzzword-it’s a life-saving rhythm.
December 28, 2025 AT 22:55 PM
the notion that caffeine is benign because it is socially sanctioned is a profound epistemological failure. we normalize substances not because they are safe, but because they are convenient. the pharmacological architecture of our bodies does not care for cultural consensus. it obeys enzymes, kinetics, and binding affinities. we are not exempt from biochemistry because we like the taste.
December 30, 2025 AT 00:32 AM
so like... what if i just... stop drinking coffee... forever... like... ever...?
December 31, 2025 AT 12:49 PM
yo i been on theophylline for 8 years and i drink 2 energy drinks a day. my doc never said nothin. now i got tremors and my heart sounds like a jackhammer. why nobody tell me? this system is broken
January 2, 2026 AT 08:14 AM
think about it: we’ve got entire industries built around selling us stimulants, then we’ve got another industry selling us drugs to fix the damage those stimulants cause. it’s capitalism as a pharmacological feedback loop. we’re not patients-we’re revenue streams. and caffeine? it’s the invisible middleman that keeps the whole rigged game spinning.
the real question isn’t ‘can i drink coffee with my meds?’ it’s ‘why does my life require this many chemical compromises just to survive?’
January 3, 2026 AT 16:16 PM
so you're telling me my morning coffee is worse than my ex? at least she didn't mess with my liver enzymes
January 4, 2026 AT 09:09 AM
thank you for this detailed post. i will now take my levothyroxine with water and wait one hour before tea.
January 6, 2026 AT 00:57 AM
ok but like... imagine if your meds were a person and coffee was the toxic ex who shows up uninvited every morning and ruins everything?? 😭☕️
January 7, 2026 AT 06:54 AM
you got this! small changes = big wins 💪☕️ (just wait 60 mins and you're golden!)
January 7, 2026 AT 07:57 AM
the study cited from JAMA Internal Medicine in April 2024 is correct. The 62% unawareness rate among patients correlates strongly with inadequate patient education protocols in primary care settings. This is not a patient failure-it is a systemic failure.
January 8, 2026 AT 09:54 AM
my grandma took warfarin for 15 years and drank one cup of coffee every morning, same time, same amount. never had an issue. consistency matters more than elimination. don’t fear coffee-respect it.
January 9, 2026 AT 12:41 PM
why are we even talking about this? just stop taking meds if you like coffee. problem solved.
January 11, 2026 AT 00:34 AM
As a certified clinical pharmacist with a Doctorate in Pharmacogenomics, I must emphasize that the CYP1A2 polymorphism is not merely a variable-it is a determinant of survival. The notion that ‘one cup is fine’ is dangerously oversimplified. Genetic testing is not optional; it is imperative.
January 11, 2026 AT 20:13 PM
they say caffeine interferes with meds but they never mention that sugar in coffee does way more damage. why is no one talking about the real villain?