Antipsychotic Treatment Decision Assistant
Treatment Decision Guide
This tool helps determine the most appropriate antipsychotic based on key factors including treatment resistance, comorbidities, monitoring capacity, side effect tolerance, and cost. Using evidence-based guidelines, it provides recommendations aligned with clinical best practices.
Patient Assessment
Ever wonder why doctors sometimes push Clozaril even though it’s famous for a handful of scary lab tests? The answer lies in its unique ability to help patients who have exhausted every other option for schizophrenia. Below we break down how Clozapine stacks up against the most commonly prescribed antipsychotics, what side‑effects to watch for, and how to decide which drug fits a particular patient.
What Is Clozapine and How Does It Work?
Clozapine is a second‑generation (atypical) antipsychotic that targets multiple neurotransmitter systems. It blocks dopamine D2 receptors while also antagonizing serotonin 5‑HT2A receptors, which helps reduce both positive and negative symptoms of schizophrenia. Unlike many newer agents, Clozapine has a high affinity for the dopamine D4 subtype, offering extra control over treatment‑resistant cases.
Because of its broad receptor profile, Clozapine also dampens glutamate release and influences histamine and muscarinic receptors. This mix explains why it can be more effective for stubborn hallucinations but also why it carries a distinct side‑effect bundle.
When Is Clozapine the Right Choice?
- Patient has failed to improve after trials of at least two other antipsychotics at adequate doses.
- Severe “negative” symptoms (social withdrawal, lack of motivation) dominate the clinical picture.
- History of frequent relapses despite good medication adherence.
Guidelines from the American Psychiatric Association (APA) and NICE list Clozapine as the gold‑standard for "treatment‑resistant schizophrenia". In a 2023 meta‑analysis of 34 randomized controlled trials, Clozapine showed a 30 % higher response rate than any other oral antipsychotic.
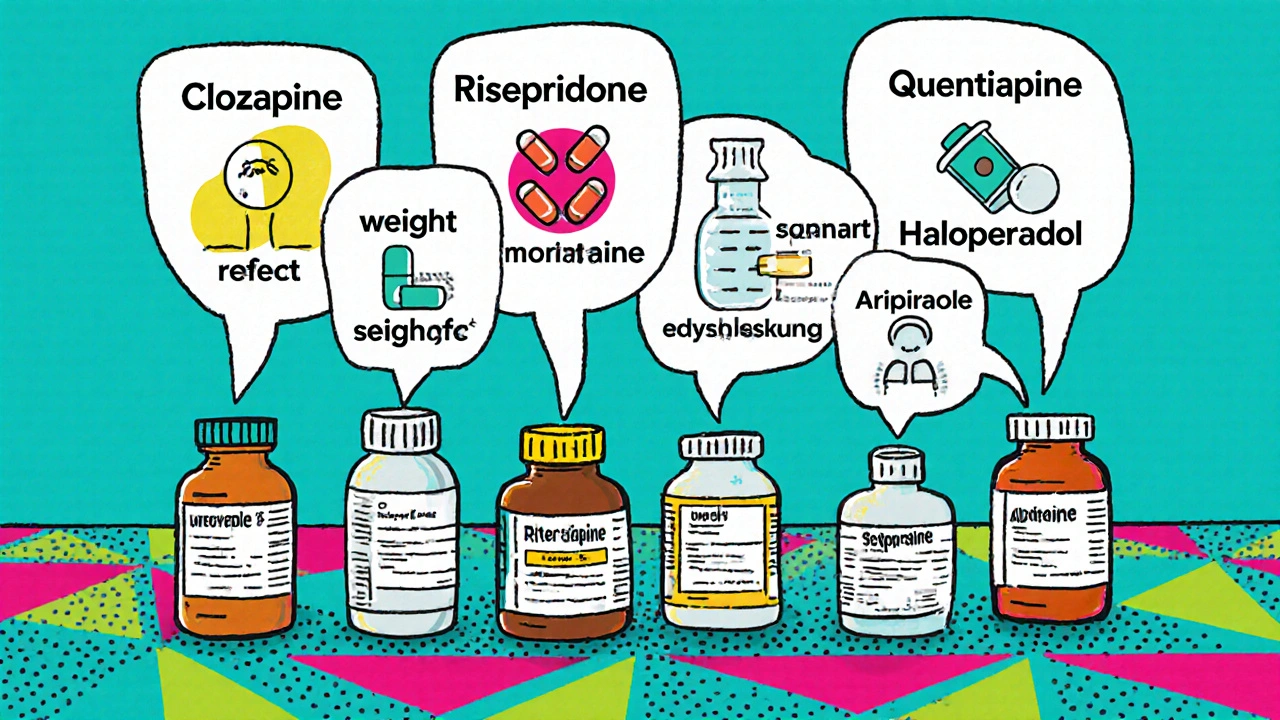
Common Alternatives: A Quick Overview
Below are the six most frequently prescribed rivals, each with its own strengths and downsides.
- Risperidone is an atypical antipsychotic that balances dopamine D2 and serotonin 5‑HT2A blockade, offering solid control over positive symptoms with moderate metabolic risk.
- Olanzapine provides strong symptom relief but is notorious for weight gain and diabetes risk.
- Quetiapine is often used for its sedating properties and is a go‑to for patients with comorbid insomnia.
- Haloperidol is a first‑generation (typical) antipsychotic; it’s cheap and potent but brings a high chance of extrapyramidal symptoms.
- Aripiprazole works as a dopamine partial agonist, reducing the risk of motor side‑effects while still tackling psychosis.
Side‑Effect Landscape: Clozapine vs the Rest
Every antipsychotic has a side‑effect profile, but they differ in severity and required monitoring.
| Drug | Typical Dose (mg/day) | Efficacy for Treatment‑Resistant Schizophrenia | Major Side Effects | Monitoring Needs |
|---|---|---|---|---|
| Clozapine | 300‑600 | High - best‑in‑class | Agranulocytosis, myocarditis, metabolic syndrome | Weekly CBC for first 6 weeks, then bi‑weekly |
| Risperidone | 2‑6 | Moderate | Prolactin elevation, mild weight gain | Baseline metabolic panel, periodic prolactin checks |
| Olanzapine | 10‑20 | High for general schizophrenia | Significant weight gain, hyperglycemia | Quarterly fasting glucose & lipid panel |
| Quetiapine | 300‑800 | Low‑moderate | Excessive sedation, orthostatic hypotension | Blood pressure monitoring, occasional labs |
| Haloperidol | 5‑20 | Moderate | Extrapyramidal symptoms, tardive dyskinesia | Movement disorder assessment every visit |
| Aripiprazole | 10‑30 | Moderate | Akathisia, insomnia | Monitor for restlessness, sleep pattern |
The table makes it clear why Clozapine is reserved for the toughest cases: its effectiveness comes with the need for rigorous blood monitoring to catch Agranulocytosis, a potentially fatal drop in white blood cells.
Decision‑Making Framework: Choosing the Right Drug
- Assess treatment resistance. If two trials at therapeutic doses have failed, move to Clozapine.
- Check patient comorbidities. Metabolic issues push clinicians toward Aripiprazole or Risperidone; cardiac history may rule out Clozapine.
- Evaluate monitoring capacity. Weekly CBCs require a clinic that can track labs reliably.
- Discuss side‑effect tolerance. Some patients prefer sedation (Quetiapine) over metabolic gain (Olanzapine).
- Consider cost and insurance. Haloperidol is cheap, but cheaper isn’t always better for long‑term outcomes.
By walking through these checkpoints, you can align the drug’s pharmacology with the patient’s lived reality.
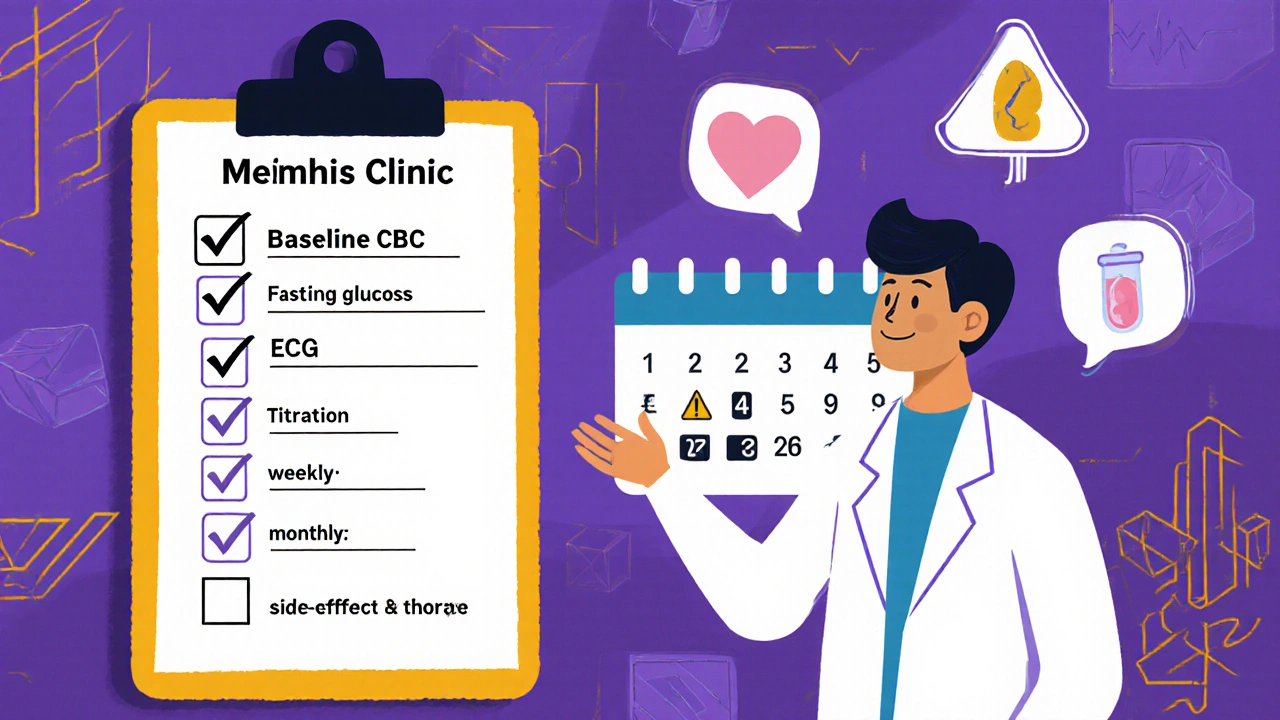
Practical Checklist for Initiating Clozapine
- Obtain baseline complete blood count (CBC), fasting glucose, lipids, and ECG.
- Enroll the patient in a national Clozapine registry (U.S. REMS, UK CLOZAPINE REMS).
- Educate the patient about daily blood draws and infection warning signs.
- Start at 12.5 mg once or twice daily; titrate up to target 300‑600 mg over 2‑4 weeks.
- Schedule CBCs: weekly for 6 weeks, then every 2 weeks up to 18 weeks, then monthly.
- Monitor weight, BMI, and fasting glucose at each visit.
- Plan for rapid discontinuation if ANC < 1500/µL; develop an alternative antipsychotic backup.
Frequently Asked Questions
Why is Clozapine called a “last‑resort” medication?
Because it’s the only drug proven to work when two other antipsychotics have already failed, but it also carries a risk of serious blood disorders that require close monitoring.
Can I switch from another antipsychotic to Clozapine overnight?
No. A cross‑taper over 1‑2 weeks is recommended to avoid withdrawal psychosis and to let the new drug reach steady state.
What are the warning signs of agranulocytosis?
Fever, sore throat, mouth ulcers, or any sign of infection should prompt an immediate CBC and a call to the prescriber.
Is Clozapine safe during pregnancy?
Data are limited, but most guidelines advise using it only if the benefits outweigh the risks, because the blood‑monitoring requirements can be harder to meet in pregnancy.
How does Clozapine compare cost‑wise to other antipsychotics?
Although the drug itself is generic and inexpensive, the required lab tests and registry fees often make the overall cost higher than most atypicals.
Can I take Clozapine with other psychiatric meds?
Yes, but caution is needed with drugs that also affect the QT interval or cause profound sedation; always coordinate with a psychiatrist.
What lifestyle changes help minimize Clozapine’s metabolic side effects?
Regular aerobic exercise, a low‑sugar diet, and routine weight checks can blunt weight gain and glucose spikes.
Choosing the right antipsychotic is never a one‑size‑fits‑all decision. Clozapine shines when other treatments have failed, but its safety demands a partnership between patient, clinician, and lab services. By weighing efficacy, side‑effect risk, and practical monitoring, you can land on the drug that offers the best chance of stability for each individual.



October 26, 2025 AT 11:23 AM
Honestly, the fact that some clinicians keep pushing Clozapine without fully addressing the blood‑test nightmares is just plain irresponsible. Patients deserve a treatment plan that doesn’t feel like a constant lab‑work nightmare, and it’s high time the medical community re‑evaluates the risk‑vs‑benefit balance.
November 3, 2025 AT 13:50 PM
From a neuropharmacological standpoint Clozapine's multi‑receptor antagonism – D2, 5‑HT2A, D4, muscarinic – provides a unique symptom‑reduction profile especially for treatment‑resistant schizophrenia 😎 its metabolic monitoring demands are a logistical hurdle however the efficacy data (OR≈1.3) justifies the regimen 📊
November 11, 2025 AT 16:17 PM
Yeah right, “justifies the regimen” while patients are stuck with weekly blood draws and a constant fear of agranulocytosis. Talk about swapping one nightmare for another, no thanks.
November 19, 2025 AT 18:43 PM
I get why the monitoring feels overwhelming – it’s a lot to ask anyone to do. Still, hearing stories from folks who finally found stability on Clozapine can be a huge relief and a reminder that the effort can pay off.
November 27, 2025 AT 21:10 PM
Totally agree! 😊 Clozapine may be a tough road, but for many it’s the only path to feeling like yourself again. Keep the conversation going, we’re all in this together! 👍
December 5, 2025 AT 23:37 PM
Clozapine works well when other meds fail. It needs blood tests, but it can help with hard‑to‑treat symptoms.
December 14, 2025 AT 02:03 AM
Considering the side‑effect profile, it’s essential to match the medication to the individual’s comorbidities and support system. Not everyone can handle the monitoring, so alternatives remain viable.
December 22, 2025 AT 04:30 AM
In the grand tapestry of psychopharmacology, Clozapine is the elusive thread one must pull to reveal the hidden pattern – assuming you’re willing to stare at the abyss of weekly CBCs while contemplating the nature of consciousness 😂.
December 30, 2025 AT 06:57 AM
I’m curious about the real‑world adherence rates when patients have to schedule weekly labs. Does the benefit in symptom reduction offset the logistical burden in everyday clinic settings?
January 7, 2026 AT 09:23 AM
Great points all around! If someone’s worried about the labs, maybe a care coordinator can help streamline the process – turning a daunting task into a manageable routine.
January 15, 2026 AT 11:50 AM
One might surmise that the ubiquitous emphasis on Clozapine’s superiority is a subtle orchestration by pharmaceutical conglomerates to monopolize the market under the guise of “treatment‑resistant” classification. Nevertheless, the data, albeit meticulously curated, still suggests a genuine therapeutic edge – or does it?
January 23, 2026 AT 14:17 PM
Let’s break this down step by step: Clozapine’s efficacy is undeniably impressive in refractory cases, yet the accompanying monitoring protocol demands a coordinated effort from both patients and providers. While some may view the weekly CBCs as onerous, it also offers an ongoing safety net, catching potential hematologic issues before they become critical. Moreover, integrating lifestyle interventions-regular exercise, balanced nutrition-can mitigate its metabolic side effects, creating a holistic treatment approach. In practice, a multidisciplinary team, consisting of psychiatrists, primary care physicians, and nursing staff, can distribute the workload, ensuring compliance without overwhelming the patient. Ultimately, the decision hinges on a nuanced risk‑benefit analysis tailored to each individual’s circumstances.
January 31, 2026 AT 16:43 PM
Clozapine is effective but requires strict monitoring it isn’t for everyone