Digoxin-Amiodarone Dose Adjustment Calculator
When starting amiodarone while taking digoxin, you must adjust the digoxin dose to prevent life-threatening toxicity. Based on current guidelines, the recommended dose adjustment depends on your kidney function.
Your adjusted digoxin dose:
Based on your GFR of mL/min, your digoxin dose should be reduced by .
Critical Guidelines
These recommendations follow the most current clinical guidelines:
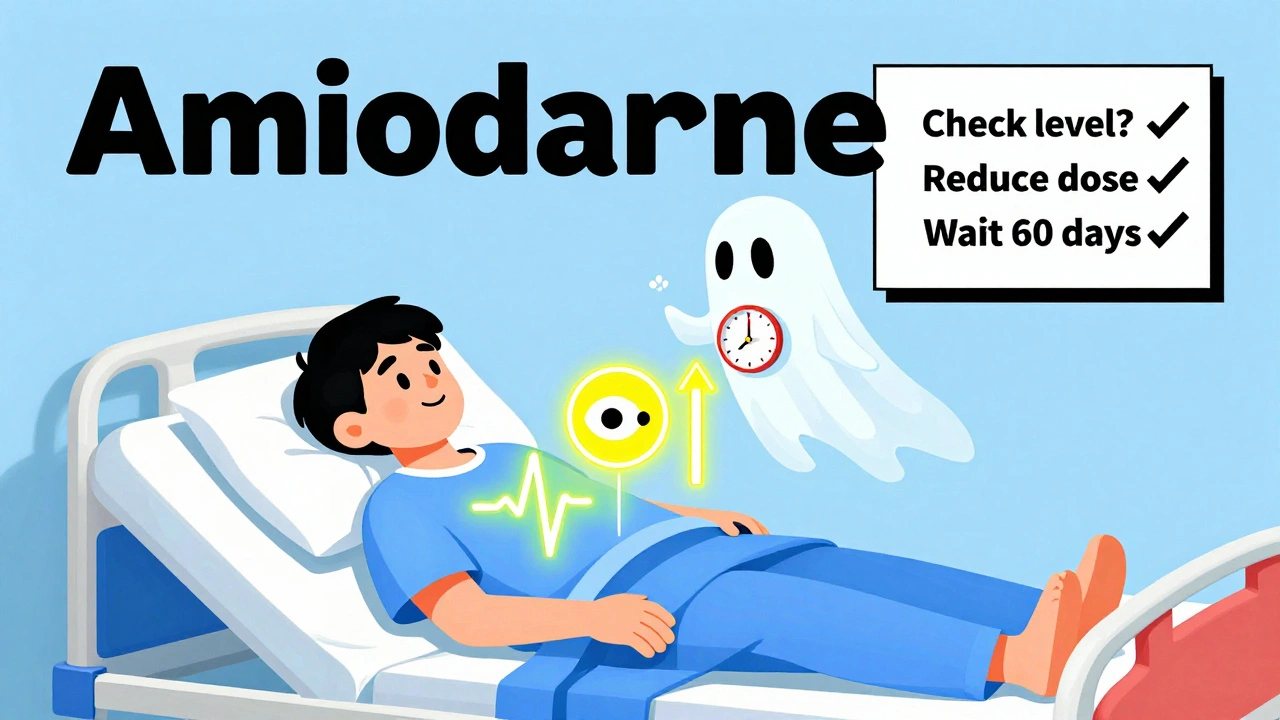
- Always check digoxin levels before starting amiodarone
- Reduce digoxin dose by 50% when starting amiodarone
- Reduce to 33% if eGFR < 50 mL/min
- Check digoxin levels again 72 hours after starting amiodarone
- Monitor levels weekly for the first month
Important Safety Warning
Forgetting to adjust your digoxin dose can lead to life-threatening toxicity. Even a small error can cause:
- Severe bradycardia (heart rate < 50 bpm)
- Hyperkalemia (potassium > 5.5 mEq/L)
- Cardiac arrest
- Increased mortality risk by 27 percentage points
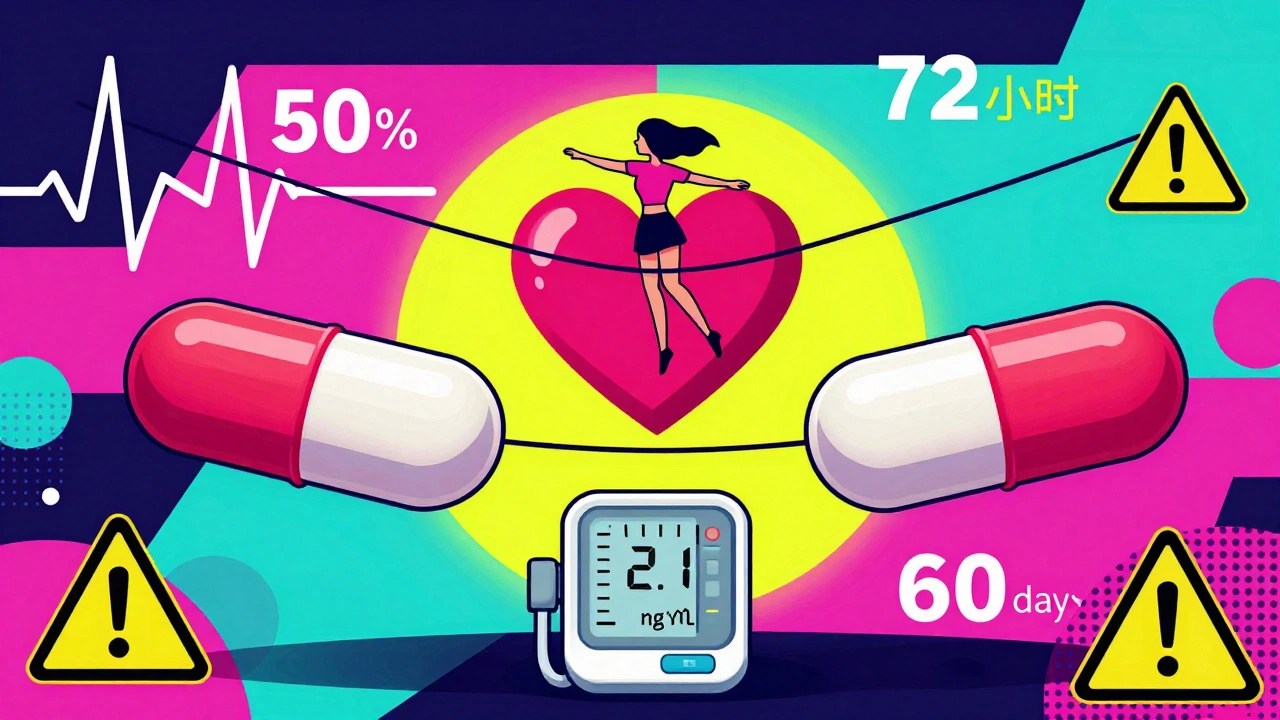
When you’re on digoxin for heart failure or atrial fibrillation, and your doctor adds amiodarone to control your rhythm, you’re walking a tightrope. Both drugs have digoxin and amiodarone are powerful, but they don’t play well together. Even a small mistake in dosing can send you to the ICU. This isn’t theoretical-it’s happening right now in hospitals and clinics across the country. In fact, studies show that nearly 60% of patients on both drugs aren’t getting their digoxin dose adjusted, and that’s why so many end up with life-threatening toxicity.
Why This Interaction Is So Dangerous
Digoxin is a cardiac glycoside. It’s been around since the 1930s, and it works by slowing down the heart’s electrical signals to control fast rhythms like atrial fibrillation. But it doesn’t take much to push it into the toxic zone. The safe range? Between 0.5 and 0.9 nanograms per milliliter in your blood. Go above 1.0, and you’re at risk. Above 2.0? That’s a medical emergency. Amiodarone, on the other hand, is a complex antiarrhythmic. It’s used when other drugs fail. But it doesn’t just work on the heart-it messes with your liver, lungs, thyroid, and, critically, how your body clears digoxin. When you take both, amiodarone blocks a protein called P-glycoprotein. This protein normally pumps digoxin out of your cells and kidneys so it can leave your body. When it’s blocked, digoxin builds up. Studies show serum levels can jump by 100% or more within days. This isn’t a slow burn. Toxicity can hit fast. One 2023 case report described a 72-year-old woman who developed potassium levels of 6.8 mEq/L (normal is 3.5-5.0) and a dangerously slow heart rate after starting amiodarone on her full digoxin dose. She ended up in the ICU for four days. She didn’t have a history of kidney disease. She didn’t take extra pills. She just didn’t get her dose lowered.How the Interaction Actually Works
The science behind this isn’t complicated, but it’s often misunderstood. Amiodarone doesn’t just increase digoxin levels-it changes how your body handles it on multiple levels:- It reduces digoxin clearance by nearly 30%, meaning your kidneys and liver can’t get rid of it as fast.
- It cuts non-renal clearance (how your body breaks it down outside the kidneys) by a third.
- It increases digoxin’s half-life from about 36 hours to over 60 hours.
- It also boosts digoxin’s absorption in the gut, so you’re taking in more of it even if the dose hasn’t changed.
What Happens When You Don’t Adjust the Dose
The consequences aren’t just theoretical. A 2021 study in Circulation: Arrhythmia and Electrophysiology found that patients on both drugs were 2.3 times more likely to be hospitalized for digoxin toxicity than those on digoxin with other common drugs like furosemide. The mortality risk? Even worse. Dr. Gregg C. Fonarow’s 2021 analysis showed that when patients kept their full digoxin dose while starting amiodarone, their 30-day death rate jumped from 8% to 35%. That’s not a typo. That’s a 27 percentage point increase in death risk. And it’s not just about heart rhythm. The 2024 Stanford study found that this combo also increases stroke risk by more than double. Why? Elevated digoxin levels appear to make blood more prone to clotting. So you’re not just risking a slow heart rate-you’re risking a stroke.
What You Should Do: The Exact Protocol
There’s no guesswork here. The guidelines are clear, and they’ve been consistent for over 40 years. Here’s what you need to do:- Check your digoxin level before starting amiodarone. Don’t assume it’s fine. Even if you’ve been stable for years, levels can drift. Get a blood test.
- Reduce your digoxin dose by 50% the day you start amiodarone. This isn’t optional. It’s mandatory. The Singh study from 1984 showed that without this step, levels rise dangerously fast. The European Heart Rhythm Association, ASHP, and UCSF all agree: cut it in half.
- Check your digoxin level again 72 hours after starting amiodarone. That’s when levels typically peak. If you’re over 0.9 ng/mL, you need another reduction.
- If you have kidney problems (eGFR under 50 mL/min), cut the dose to 33% of your original dose. Your kidneys are already struggling to clear digoxin. Adding amiodarone without further reduction is asking for trouble.
- Keep checking levels every week for the first month. Amiodarone’s effects build slowly. You might be fine at day 3, but not at day 14.
Why So Many Doctors Still Get It Wrong
You’d think this would be common knowledge by now. But a 2022 study across 15 U.S. hospitals found that only 44% of patients had their digoxin dose reduced when amiodarone was started. In community hospitals? It was worse-68% of patients were left on full doses. Why? Several reasons:- Doctors assume the patient’s current digoxin level is safe, so they don’t check it.
- They think, “She’s been on digoxin for years-she’s fine.” But stability doesn’t mean immunity.
- Amiodarone is often started in an emergency-like a new-onset rapid AF-and dose adjustments get overlooked in the rush.
- Many clinicians don’t realize the interaction lasts for months after stopping amiodarone.
What’s Changing in 2025
The tide is turning. New guidelines from the European Society of Cardiology in 2024 now recommend avoiding digoxin altogether in patients with atrial fibrillation who are likely to need amiodarone. Beta-blockers or diltiazem are safer for rate control. The DIG-AMIO trial (NCT05217891), currently enrolling patients, is comparing 50% vs. 33% digoxin dose reduction with amiodarone. Results are expected in late 2025. But you don’t need to wait for those results. The evidence is already overwhelming. Health systems are catching up, too. The Veterans Health Administration saw a 41% drop in digoxin toxicity after adding automated EHR alerts that pop up when both drugs are prescribed. Some hospitals now require pharmacist sign-off before amiodarone is dispensed to patients on digoxin.What to Watch For: Signs of Toxicity
If you’re on both drugs, know the red flags:- Nausea, vomiting, or loss of appetite
- Blurred vision, yellow or green halos around lights
- Unexplained fatigue or dizziness
- Heart rate below 50 beats per minute
- Irregular heartbeat-especially new pauses or skipped beats
- High potassium levels (above 5.5 mEq/L)
Bottom Line: Don’t Guess. Act.
This interaction is one of the most dangerous in cardiology. It’s not rare. It’s not obscure. It’s common, predictable, and preventable. You don’t need to be a specialist to understand it. You just need to know: digoxin and amiodarone together require a 50% digoxin dose reduction-no exceptions. If you’re a patient: Ask your doctor, “Will my digoxin dose be lowered when I start amiodarone?” If you’re a clinician: Write the order for the reduction before you even write the amiodarone script. Use the EHR alert if it’s there. If it’s not, create your own checklist. The data doesn’t lie. The cases don’t lie. The deaths don’t lie. This isn’t about being careful. It’s about being exact.Can I still take digoxin if I need amiodarone?
Yes, but only if you reduce your digoxin dose by at least 50% when starting amiodarone. Never keep the same dose. Monitor digoxin levels at 72 hours after starting amiodarone and again at one week. If you have kidney problems, reduce digoxin to 33% of your original dose. This combination is high-risk, but manageable with strict protocol.
How long does the interaction last after stopping amiodarone?
Amiodarone and its active metabolite, desethylamiodarone, can stay in your body for up to 60 days after you stop taking it. That means digoxin levels remain elevated during this time. Do not increase your digoxin dose until at least two months after discontinuing amiodarone, and only after checking your serum level.
Is digoxin still used today, or should I avoid it?
Digoxin is still used, especially in heart failure patients with atrial fibrillation who don’t respond to beta-blockers or calcium channel blockers. But its use has declined because of interaction risks like this one. For many patients with atrial fibrillation, safer alternatives like metoprolol or diltiazem are now preferred, especially if amiodarone might be needed later.
Can I check my digoxin level at home?
No. Digoxin levels require a blood test drawn from a vein and analyzed in a lab. Home testing isn’t available. If you’re on both drugs, your doctor should schedule a blood test before starting amiodarone and again 72 hours after. Don’t skip these tests-they’re critical.
What if my doctor doesn’t know about this interaction?
Bring the guidelines. Print out the 2022 European Heart Rhythm Association recommendation or the ASHP guideline. Say, “I’ve read that digoxin must be reduced by 50% when starting amiodarone. Can we adjust my dose now?” If your doctor is unsure, ask to speak with a pharmacist or cardiac specialist. This is a well-documented, high-risk interaction that every cardiologist is trained on.
Are there safer alternatives to amiodarone?
Yes. For atrial fibrillation, dronedarone is an option-but it’s not safer with digoxin and has its own risks. Flecainide or propafenone may work if you don’t have structural heart disease. For rate control, beta-blockers like metoprolol or calcium channel blockers like diltiazem are preferred. If you’re on digoxin and need rhythm control, talk to your doctor about alternatives to amiodarone.


December 3, 2025 AT 10:45 AM
Wow. Another ‘I read a study’ post pretending to be medical advice. Newsflash: if your doctor doesn’t know this, they shouldn’t be prescribing anything. 🤦♂️
December 4, 2025 AT 22:23 PM
It’s staggering how deeply embedded this oversight is in clinical practice. The pharmacokinetic interplay isn’t just a footnote-it’s a seismic shift in clearance dynamics. Amiodarone’s half-life dwarfs digoxin’s, and yet we treat it like a temporary fix. The human cost isn’t just statistical; it’s the 72-year-old woman who didn’t get her dose lowered because someone assumed ‘stable’ meant ‘safe.’ We’re not managing drugs-we’re managing risk, and we’re failing at it systematically.
December 6, 2025 AT 15:50 PM
bro this is wild. i had a uncle on both drugs and he got hospitalized. no one told us to reduce digoxin. we just thought he was getting older. sad.
December 7, 2025 AT 12:28 PM
Oh great. Another ‘follow the protocol’ lecture from someone who thinks medicine is a checklist and not a living, breathing art form. What about individual variation? What about patient autonomy? You want everyone on a 50% reduction like it’s a factory line? The real danger here is blind adherence to guidelines without clinical judgment. 🤖💊
December 9, 2025 AT 12:18 PM
So let me get this straight - we’re supposed to reduce digoxin by 50%... but only if you’re lucky enough to have a doctor who remembers to check labs? 😂 I mean, my PCP still thinks ‘EKG’ is a brand of headphones. This is why I bring printed guidelines to every appointment. 📄✨
December 10, 2025 AT 12:22 PM
India also sees this. Many doctors forget. Patient dies. Family blames God. No one blames the system.
December 11, 2025 AT 18:16 PM
Pharmacodynamic displacement via P-glycoprotein inhibition is the primary driver of digoxin accumulation, compounded by reduced renal excretion and altered tissue distribution. The clinical implications are non-trivial and demand tiered monitoring protocols with therapeutic drug monitoring (TDM) as a mandatory component. Failure to implement this constitutes a breach of standard of care.
December 13, 2025 AT 16:52 PM
So… we’re just supposed to trust that some overworked resident in a 3am shift will remember to adjust a dose that’s been stable for 12 years? And if they don’t? The patient dies. And then we all get a nice email from the hospital about ‘continuous quality improvement.’ 💀
December 15, 2025 AT 01:55 AM
I’m so tired of being told to ‘just ask’ when the system is rigged. My mom almost died from this. They didn’t even check her levels for three weeks. Now I’m the one who has to Google everything. And I’m not even a nurse. I’m just a daughter who cried in the parking lot after the ICU visit. 😔
December 15, 2025 AT 22:30 PM
You got this. Knowledge is power. Share this with your doctor. You’re already ahead of 90% of patients. 💪❤️
December 16, 2025 AT 17:01 PM
The institutional inertia surrounding this interaction is not merely negligent-it is ethically indefensible. The evidence base is robust, the guidelines are unequivocal, and yet the variance in practice across tertiary and community hospitals remains staggering. The introduction of EHR-based alerts, as demonstrated by the VA, is not merely beneficial-it is a moral imperative. To continue prescribing without protocol-driven intervention is to participate in a system that commodifies human life.
December 16, 2025 AT 23:06 PM
This is such an important post. Seriously, if you're on digoxin and your doc is about to start amiodarone-don't wait. Ask for the dose adjustment. Print this out. Bring it. You're not being annoying-you're saving your life. ❤️
December 17, 2025 AT 15:39 PM
my dr told me ‘it’s fine’ when i asked about the interaction. i just started taking it anyway. now i’m scared to sleep. why does everyone act like this is normal??
December 18, 2025 AT 01:01 AM
It is not hyperbolic to assert that this pharmacological interaction constitutes a structural failure of medical education and institutional oversight. The persistence of this preventable mortality vector, despite decades of peer-reviewed literature and consensus guidelines, suggests a pathological dissonance between evidence-based medicine and clinical practice. The absence of mandatory pharmacist intervention or automated EHR alerts in 68% of community settings is not an oversight-it is a systemic betrayal.
December 19, 2025 AT 14:08 PM
Bro. This is why I love medicine. Real science. Real stakes. I’ve seen this exact scenario play out-patient on digoxin for years, gets amiodarone for new AFib, ends up in the ER with VTach and potassium at 6.9. No one touched the digoxin. We gave digibind, put them on a drip, and they lived. But it was too close. Don’t wait. Cut the dose. Check the level. Repeat. This isn’t theory-it’s your next patient. 🙏
December 19, 2025 AT 22:06 PM
amiodarone digoxin interaction is well known why are we still talking about this its basic pharma
December 20, 2025 AT 20:01 PM
my cousin got this wrong and ended up in the hospital. i printed this out and gave it to my mom’s dr. she actually listened. i’m so proud. 🙌
December 22, 2025 AT 17:03 PM
So if I’m understanding this right - amiodarone sticks around for months, so even if you stop it, you still need to keep digoxin low for 60+ days? 😳 I didn’t realize it was this long-term. That’s wild. Thanks for spelling this out. I’m sharing this with my whole family. ❤️
December 24, 2025 AT 12:06 PM
It’s profoundly disturbing that this interaction remains so poorly managed despite being documented since the 1980s. The persistence of this error speaks not to ignorance, but to institutional complacency. The fact that 68% of community hospitals still fail to reduce digoxin doses indicates a deeper pathology: the normalization of preventable harm. This is not a clinical error-it is a moral failure, and until clinicians are held accountable-not just through guidelines, but through liability, audit, and consequence-we will continue to bury patients who never had a chance.