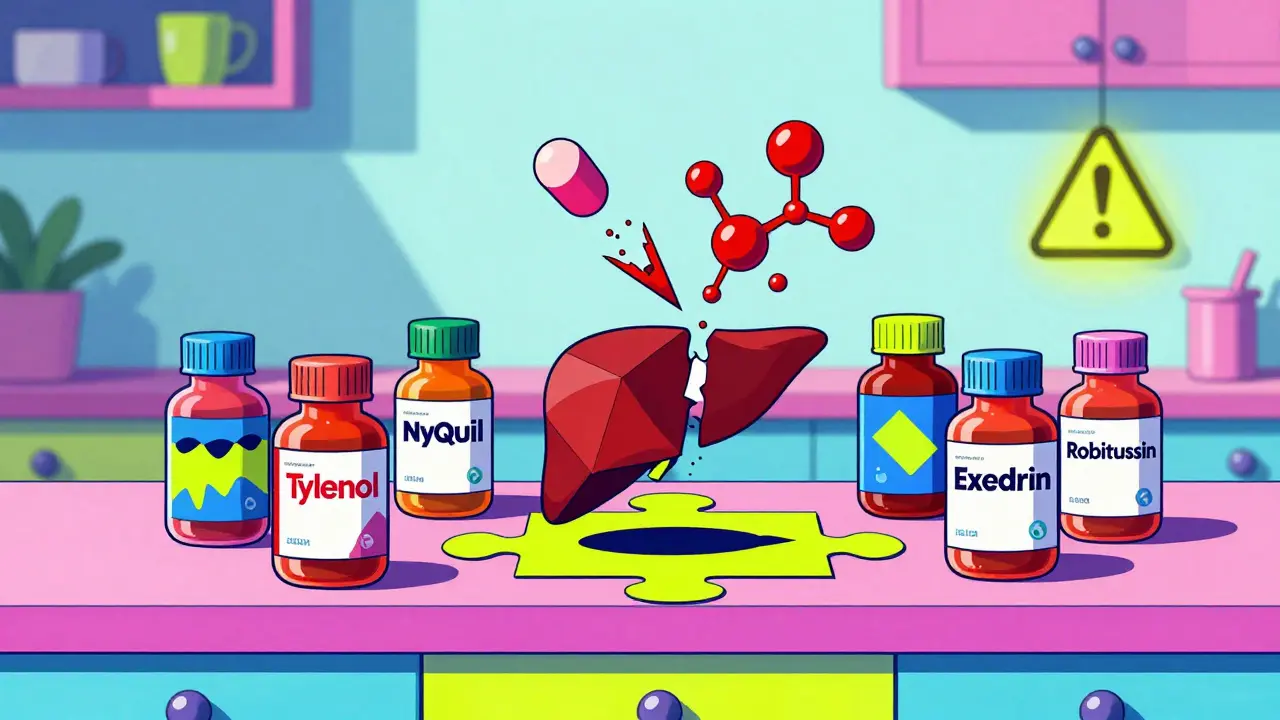
Every year, tens of thousands of people end up in the emergency room because they took what they thought was a safe, over-the-counter pain reliever. The culprit? Acetaminophen. It’s in more than 600 products-from Tylenol to cold medicines, sleep aids, and even some prescription pills. Most people don’t realize they’re stacking doses. And that’s how liver damage happens-quietly, and often too late.
Why Acetaminophen Is a Silent Threat
Acetaminophen (also called paracetamol) is not dangerous when used correctly. In fact, it’s the safest OTC pain reliever for people with liver disease-if you stick to the limits. The problem isn’t the drug itself. It’s how easily you can accidentally overdose.
Here’s how it works: Your liver breaks down acetaminophen into harmless byproducts. But when you take too much, your liver runs out of its natural defense-glutathione. That’s when a toxic compound called NAPQI builds up and starts killing liver cells. This isn’t theoretical. In the U.S., acetaminophen causes more than 56,000 emergency visits and nearly 500 deaths each year, according to CDC data from 2023.
The scary part? Most of these cases aren’t suicide attempts. They’re mistakes. Someone takes Tylenol for a headache, then a cold medicine later that night-both contain acetaminophen. By bedtime, they’ve hit 4,000 mg without even trying.
What’s the Real Safe Dose?
The old rule-4,000 mg per day-is no longer the gold standard for everyone. The FDA updated guidelines in 2021 and now recommends a max of 3,250 mg per day for prescription combo products. For OTC use, the label still says 4,000 mg, but experts say that’s too high for many people.
Here’s what you should actually follow:
- Healthy adults: Don’t exceed 3,000 mg per day. That’s six 500 mg pills. Never take more than 1,000 mg per dose.
- People with liver disease (fatty liver, hepatitis, cirrhosis): Limit to 2,000 mg per day-no more than four 500 mg pills. Some doctors recommend even less.
- If you drink alcohol: Cut your limit in half. Even one drink a day can lower your safe threshold to 2,000 mg or less. Alcohol and acetaminophen together are a dangerous mix.
And don’t assume “extra strength” means you can take fewer pills. Two extra-strength Tylenol (1,000 mg total) is still half your daily limit. One cold tablet? That’s another 325 mg. You’re already halfway there before you even think about pain.
Hidden Acetaminophen Is the Biggest Risk
You won’t find acetaminophen listed as “acetaminophen” on every label. It’s often hiding under names like “APAP,” “acetaminophen,” or “paracetamol.” But more importantly, it’s in combo products you wouldn’t suspect.
Check these common products:
- Excedrin (migraine relief)
- DayQuil, NyQuil, Theraflu
- Robitussin Multi-Symptom
- Prescription painkillers like Vicodin, Percocet, Norco
- Some sleep aids like Tylenol PM
A 2022 FDA study found that 25% of unintentional overdoses came from people taking multiple cold and flu products without realizing they all contained acetaminophen. One person takes NyQuil for a cough, then takes Tylenol for a fever. Boom-overdose.
Here’s a simple trick: Before you take any new medicine, look at the “Active Ingredients” section on the Drug Facts label. If it says acetaminophen, APAP, or paracetamol-write it down. Then add up everything you’ve taken that day.

NSAIDs Aren’t Always Safer
Many people switch to ibuprofen or naproxen thinking they’re avoiding liver risks. But that’s not the full story. NSAIDs like Advil, Aleve, and Motrin are easier on the liver-but harder on your stomach, kidneys, and heart.
According to GoodRx’s 2023 analysis, diclofenac is one of the most likely NSAIDs to cause liver injury, though it’s rare. More common? Stomach bleeding, kidney damage, and high blood pressure. If you have existing liver disease, NSAIDs can make kidney problems worse, which then puts more stress on your liver.
For people with liver conditions, topical NSAIDs (gels or patches applied to the skin) are a better option. They don’t go through the liver at all. Studies from Cary Gastroenterology in 2024 show they’re just as effective for joint and muscle pain-with almost zero liver impact.
What Are the Warning Signs?
Liver injury doesn’t come with a siren. It creeps in. You might feel fine one day, then suddenly feel sick the next.
Watch for these symptoms, especially within 24-72 hours of taking too much acetaminophen:
- Nausea or vomiting
- Loss of appetite
- Dark urine
- Clay-colored stools
- Jaundice (yellow skin or eyes)
- Pain in the upper right side of your belly
- Extreme fatigue
The National Institute of Diabetes and Digestive and Kidney Diseases found that 93% of acetaminophen-related liver failures show these signs. If you notice even one of these after taking OTC pain meds-get help immediately. Don’t wait. Don’t assume it’s “just a stomach bug.”

What to Do If You Think You’ve Overdosed
If you’ve taken more than the recommended dose-even if you feel fine-call poison control or go to the ER. Time matters.
The antidote, N-acetylcysteine (NAC), works best if given within 8 hours of overdose. After 16 hours, its effectiveness drops sharply. Many people wait because they feel okay. That’s the trap.
Even if you’re unsure-call. Poison control (1-800-222-1222 in the U.S.) doesn’t judge. They just help. And they can tell you if you’re at risk based on how much you took and when.
How to Stay Safe Long-Term
Prevention is simple. You just need to be smarter about what you take.
- Use a pill organizer. Fill it with your daily meds. Mark the max dose for acetaminophen. No guesswork.
- Keep a medication diary. Write down every pill you take-name, dose, time. Include vitamins and supplements. Some herbal products contain hidden liver toxins.
- Read every label. Even if you’ve used the product before. Formulas change.
- Avoid alcohol completely. If you’re taking acetaminophen regularly, skip the wine, beer, or spirits. No exceptions.
- Ask your pharmacist. When you pick up a new prescription or OTC product, ask: “Does this have acetaminophen?”
- Consider non-drug options. For chronic pain, physical therapy, heat/cold packs, acupuncture, or cognitive behavioral therapy are safer and often more effective long-term. The American Liver Foundation now recommends these as first-line treatments.
There’s also new tech helping people stay safe. Companies like 23andMe now offer genetic tests that can show if you have a variation in the enzyme that breaks down acetaminophen. Some people naturally produce less glutathione-and are at higher risk even at normal doses. If you have a family history of liver problems, this test could be life-saving.
What’s Changing in 2026?
Regulators are catching up. Since 2022, all OTC acetaminophen products in the U.S. must have a bold “Liver Warning” on the front label. The instructions now say “Do not exceed 4,000 mg daily”-clearly printed.
Studies from Johns Hopkins show this simple change reduced unintentional overdoses by 21%. But adult cases are still too high. The goal now is to push limits even lower-especially for older adults and those with chronic conditions.
The NIH is investing $47 million through 2028 to develop new pain relievers that don’t rely on liver metabolism. The future of pain management might be topical, inhaled, or nerve-targeted-no pills needed.
Until then, your best defense is knowledge. Acetaminophen isn’t a villain. It’s a tool. And like any tool, it’s dangerous in the wrong hands-or the wrong dose.
Can I take acetaminophen if I have fatty liver disease?
Yes-but only up to 2,000 mg per day, and never with alcohol. Fatty liver makes your liver more vulnerable to damage. Even normal doses can be risky. Always check with your doctor before taking any pain reliever regularly.
Is Tylenol safer than ibuprofen for the liver?
Yes, acetaminophen is generally safer for the liver than NSAIDs like ibuprofen-if you don’t exceed the dose. But NSAIDs are harder on your kidneys and stomach. For people with liver disease, acetaminophen at low doses is still the preferred choice. Topical NSAIDs are even safer for the liver.
How long does it take for acetaminophen to damage the liver?
Liver damage can start within hours of an overdose, but symptoms usually appear 24 to 72 hours later. That’s why people think they’re fine-they’re not. The damage is happening silently. If you’ve taken too much, don’t wait for symptoms. Get help right away.
Can I take acetaminophen while drinking alcohol occasionally?
No. Even one drink can increase your risk of liver injury. Alcohol and acetaminophen together overwhelm your liver’s ability to detoxify. The safe dose drops from 4,000 mg to as low as 2,000 mg-and even that’s risky. If you drink, avoid acetaminophen entirely.
Are there natural alternatives to OTC pain relievers?
Yes. For mild to moderate pain, try heat packs, cold therapy, physical therapy, acupuncture, or mindfulness techniques. Studies show these can reduce reliance on pills. For chronic pain, cognitive behavioral therapy (CBT) has been proven to improve pain tolerance without any liver risk.


January 24, 2026 AT 01:26 AM
I had no idea acetaminophen was in so many things. I took NyQuil last week for my cold and then Tylenol for my headache... now I'm terrified. Thanks for the warning.
January 25, 2026 AT 16:53 PM
This is exactly why pharmacists should be required to ask about OTC meds during every visit. I work in a clinic and I see this every week. People don't realize they're doubling up. The 3,000 mg cap for healthy adults is the real sweet spot.
January 26, 2026 AT 20:26 PM
I'm just saying... what if this is all a pharmaceutical scam? 😳 They make you think it's safe then BAM liver failure. I mean... why else would they hide it in 600 products? #WakeUpSheeple
January 28, 2026 AT 19:10 PM
Thank you for this comprehensive overview. In India, paracetamol is often sold without prescription and consumed casually. This information could save many lives here.