Organ-Specific Medication Risk Checker
Personal Risk Assessment
Answer these questions to determine your risk of organ damage from medications.
Why Some Medicines Hurt One Organ But Not Others
Not all drugs affect the body the same way. One pill might wreck your liver, another could mess with your kidneys, and a third might throw your heart rhythm out of whack - even if they’re all used to treat completely different conditions. This isn’t random. It’s biology. Your organs have unique jobs, unique enzymes, and unique vulnerabilities. When a drug hits the wrong spot, the damage doesn’t spread evenly. It targets what it’s built to attack - or accidentally stumbles into.
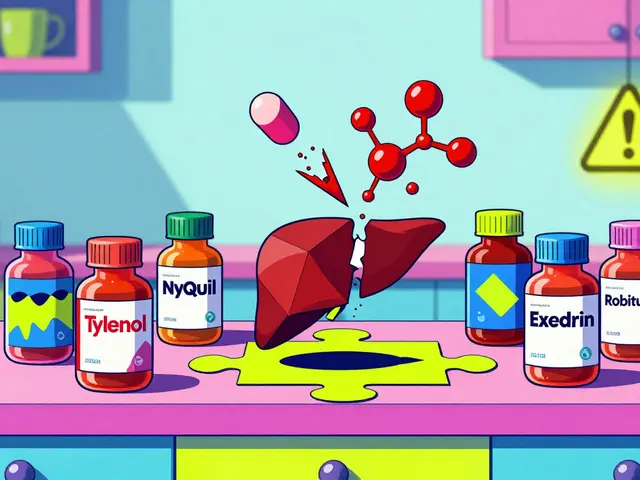
Take acetaminophen. It’s in hundreds of painkillers. Safe at the right dose. But take too much - even just 10 grams in one go - and your liver starts dying. Why? Because your liver breaks it down into a poison called NAPQI. Normally, your body neutralizes it with glutathione. But when you overdose, that buffer runs out. NAPQI starts eating liver cells alive. In the U.S., this causes over 500 deaths every year. And most people never see it coming. They just feel tired, nauseous, maybe a little off. By the time they go to the ER, it’s often too late.
Liver: The Silent Victim
The liver is the body’s chemical factory. It processes everything you take - pills, alcohol, supplements. That makes it the most common target for drug damage. About 60% of drug-induced liver injuries happen because of toxic byproducts made during metabolism. Cytochrome P450 enzymes, which are supposed to detoxify, sometimes turn safe drugs into killers.
Statins, used to lower cholesterol, cause liver enzyme spikes in 0.5% to 2% of users. Most of the time, it’s harmless. But if your ALT levels jump more than three times the normal limit - and your bilirubin climbs too - doctors will pull the plug on the drug. That’s the rule from the American Association for the Study of Liver Diseases. Some people carry a genetic variant in the SLCO1B1 gene. If you have it, your risk of liver damage from statins goes up 4.5 times. Genetic testing isn’t routine yet, but it’s coming.
Isoniazid, a tuberculosis drug, is another silent killer. Up to 20% of users get elevated liver enzymes. Most don’t feel anything. But 1-2% develop serious hepatitis. Risk spikes if you’re over 50, drink alcohol, or have slow acetylator genes. That’s why doctors check liver tests every few weeks during treatment. Fatigue, dark urine, yellow eyes - these aren’t just signs. They’re red flags.
Kidneys: The Overworked Filter
Your kidneys don’t just make urine. They filter 120-150 quarts of blood every day. That’s a lot of pressure. And many drugs don’t care. They get sucked right into kidney cells and wreck them from the inside.
Aminoglycosides like gentamicin are classic offenders. Up to half of people on long-term doses get kidney damage. The drug latches onto receptors on kidney tubules, then builds up like rust inside the cells. Mitochondria shut down. Cells die. It’s often silent until creatinine rises in a blood test. By then, damage may be permanent.
NSAIDs like ibuprofen are even sneakier. They cut blood flow to the kidneys by blocking protective prostaglandins. In older adults, they’re responsible for 15% of acute kidney injuries. Most people don’t realize they’re at risk. They pop pills for back pain, arthritis, headaches - and never think about their kidneys. The National Kidney Foundation found that 44% of patients with NSAID-related kidney damage had no symptoms until their bloodwork showed trouble.
Contrast dye used in CT scans can also fry kidneys. In healthy people, risk is low - 1-6%. But if you already have kidney disease, that jumps to 50%. Vancomycin, a powerful antibiotic, becomes dangerous when blood levels creep above 15 mg/L. Each 5 mg/L increase raises kidney injury risk by 30%. Doctors now track trough levels like a hawk.
Heart: When the Rhythm Breaks
Your heart doesn’t just pump. It beats with electrical precision. Drugs can throw that rhythm off - sometimes fatally.
Antibiotics like fluoroquinolones (ciprofloxacin, levofloxacin) increase the risk of aortic aneurysms by 31%. The exact reason? They weaken collagen in blood vessel walls. It’s not immediate. It builds over weeks. If you’re on one of these for a sinus infection, your arteries are quietly deteriorating.
Chemo drugs like doxorubicin are worse. They cause heart failure not by killing cells outright, but by generating free radicals that destroy heart muscle mitochondria. After 450-500 mg/m² of cumulative dose, 26% of patients develop heart failure. That’s why oncologists do echocardiograms every few months during treatment. If your ejection fraction drops below 45%, they stop the drug - no exceptions.
Antipsychotics like haloperidol and ziprasidone can lengthen the QT interval - the time between heartbeats. Too long, and you risk torsades de pointes, a deadly arrhythmia. Ziprasidone adds 16.4 milliseconds on average. Risperidone? Only 6.4. That’s why doctors check ECGs before and after starting these drugs. And why you should never mix them with other QT-prolonging meds like certain antibiotics or antidepressants.
Immune checkpoint inhibitors - cancer drugs that boost your immune system - can cause myocarditis. It’s rare: less than 1% of users. But when it happens, 40-50% die. Symptoms start fast - chest pain, shortness of breath, fatigue - often within 90 days of starting treatment. The FDA’s Sentinel system flagged this signal in 2018. Now, hospitals monitor patients like they’re ticking bombs.
Brain and Nerves: The Hidden Damage
Neurologic side effects are often overlooked. You don’t feel them until it’s too late.
Cisplatin, a chemo drug, causes permanent nerve damage in 30-70% of patients. It starts with numbness in fingers and toes. Then comes tingling. Then pain. It’s called peripheral neuropathy. Oxaliplatin is even weirder - it triggers sudden, painful spasms when you touch something cold. A glass of ice water can send you into a cramp. That’s not a side effect. It’s a neurological emergency.
Proton pump inhibitors (PPIs) like omeprazole are everywhere. People take them for years for heartburn. But long-term use - over 4.4 years - raises dementia risk by 21%. Why? Maybe they reduce vitamin B12 absorption. Maybe they mess with brain proteins. We don’t fully know. But the data is clear: don’t take them longer than you need to.
Phenytoin, an old epilepsy drug, causes cerebellar atrophy in up to 40% of long-term users. The cerebellum controls balance and coordination. Patients start stumbling. Their speech gets slurred. Their hands shake. It’s irreversible. And it happens even when blood levels are "within range." Dose matters - but so does time.
Immune checkpoint inhibitors can also attack nerves. They’ve been linked to Guillain-Barré syndrome, myasthenia gravis, and encephalitis. These are rare - under 0.5% combined - but deadly. If you start feeling weakness, double vision, or trouble swallowing after starting immunotherapy, get help immediately.
What You Can Do: Prevention Is Everything
You can’t always avoid these risks. But you can reduce them.
- Know your meds. Ask your doctor: "Which organs does this affect?" Don’t assume it’s safe just because it’s prescribed.
- Track symptoms. Fatigue, nausea, dark urine? Liver. Swelling in legs, less urine? Kidneys. Chest pain, fluttering heart? Heart. Numbness, dizziness, confusion? Brain. Don’t wait.
- Get tested. Liver enzymes, creatinine, eGFR, ECG - these aren’t just routine checks. They’re life-saving tools. If you’re on long-term meds, ask for them every 3-6 months.
- Don’t mix. NSAIDs + diuretics + ACE inhibitors = kidney disaster. Statins + grapefruit = liver overload. Always tell your pharmacist what else you’re taking.
- Genetics matter. If you’ve had a bad reaction before, tell your doctor. You might have a hidden gene variant that makes you vulnerable.
There’s new hope, too. In 2023, the FDA approved the first blood test that detects liver damage before ALT rises - using microRNA-122 and keratin-18. It spots injury 3-5 days earlier. Kidney biomarkers like TIMP-2 and IGFBP7 are close behind. These aren’t science fiction. They’re here.
When to Stop - And When to Push Forward
Not every side effect means you must quit the drug. Sometimes, the benefit outweighs the risk. But you need to know the thresholds.
- Liver: Stop if ALT >5x normal, or >3x normal with bilirubin >2x normal.
- Kidneys: Hold meds if eGFR drops below 30. Adjust doses if it’s below 60.
- Heart: Stop anthracyclines if LVEF falls below 45% or drops more than 15 points.
- Neurologic: If you develop new weakness, numbness, or confusion - stop and get evaluated. Don’t wait.
These aren’t guesses. They’re guidelines from the American Association for the Study of Liver Diseases, KDIGO, and the European Society of Cardiology. Follow them.
Drug development is getting smarter. Organ-on-chip tech now predicts liver and kidney toxicity with 92% accuracy before a drug ever hits humans. AI systems are scanning millions of patient records to catch hidden dangers. The future isn’t just about treating disease - it’s about avoiding harm before it starts.
Frequently Asked Questions
Can organ-specific side effects be reversed?
Sometimes, yes - if caught early. Liver damage from acetaminophen can heal if you stop the drug and get N-acetylcysteine within 8 hours. Kidney injury from NSAIDs often improves after stopping the medication and rehydrating. But nerve damage from chemo, heart muscle loss from doxorubicin, or brain changes from long-term PPIs are often permanent. The key is catching it before the damage becomes irreversible.
Are over-the-counter drugs safe for my liver and kidneys?
Not always. Acetaminophen is the #1 cause of acute liver failure in the U.S. NSAIDs like ibuprofen and naproxen are leading causes of kidney injury in older adults. Even "natural" supplements like kava, green tea extract, and black cohosh have caused liver failure. Just because it’s sold without a prescription doesn’t mean it’s harmless. Always check with your doctor before taking them long-term.
Why do some people get side effects and others don’t?
Genetics play a huge role. Variants in genes like SLCO1B1 (statins), NAT2 (isoniazid), and MATE1/OCT2 (kidney drugs) change how your body handles medications. Age matters too - older adults have less kidney function and slower metabolism. Other meds you take, alcohol use, and existing conditions like diabetes or high blood pressure also increase risk. It’s not bad luck. It’s biology.
How often should I get blood tests if I’m on long-term medication?
For liver-affecting drugs like statins or anticonvulsants, get liver enzymes checked every 3 months for the first year, then every 6-12 months if stable. For kidney-affecting drugs like NSAIDs or diuretics, check creatinine and eGFR every 3-6 months. For heart-affecting drugs like doxorubicin, echocardiograms every 2-3 months are standard. Don’t wait for symptoms - test before damage shows up.
Is there a way to protect my organs from drug damage?
You can’t fully shield yourself, but you can reduce risk. Stay hydrated - especially with NSAIDs and contrast dyes. Avoid alcohol with liver-affecting drugs. Don’t take more than one NSAID at a time. Ask about alternatives - for example, celecoxib may be safer for kidneys than ibuprofen. And if you’re on multiple meds, ask your pharmacist for a medication review. Many side effects happen because of interactions, not the drug alone.
Next Steps: What to Do Right Now
If you’re taking any prescription or long-term OTC medication:
- Write down every drug, supplement, and herb you take - including doses and how long you’ve been on them.
- Ask your doctor: "Which organs does this affect? What signs should I watch for?" Write down the answer.
- Check your last blood test results. Do you know your ALT, creatinine, and eGFR numbers? If not, request them.
- If you’ve had unexplained fatigue, swelling, chest discomfort, or numbness - don’t ignore it. Call your doctor. Bring your list.
- Set a reminder for your next blood test or checkup. Don’t wait for symptoms to appear.
Organ damage doesn’t shout. It whispers. And if you’re not listening, it gets louder - until it’s too late. Knowledge isn’t just power. It’s protection.


October 30, 2025 AT 11:06 AM
I've been on statins for 8 years and never knew about SLCO1B1. My doc never mentioned genetic testing. Guess I got lucky. But now I'm gonna ask for that blood panel next visit. 🤔
October 31, 2025 AT 14:51 PM
People think OTC means safe. Lol. Acetaminophen kills more than heroin in this country and no one talks about it. You think your liver's invincible until it's not.
November 1, 2025 AT 15:53 PM
NSAIDs are the real villain here. Not the meds. Not the doctors. YOU. You pop ibuprofen like candy. Then you wonder why your kidneys give out at 55.
November 1, 2025 AT 21:04 PM
This is why I always ask my pharmacist to do a med review. No judgment. Just safety. 🙌 If you're on more than 5 pills, you owe it to yourself to get this done. Seriously.
November 2, 2025 AT 11:37 AM
It's not just biology. It's capitalism. Pharma doesn't care about your liver because your liver doesn't buy stock. They sell the pill, not the warning. The system is designed to ignore the slow bleed until it's too late.
November 4, 2025 AT 07:22 AM
They're hiding the truth. The microRNA test? It's been available since 2021. Why isn't it mandatory? Because the FDA is in bed with Big Pharma. They don't want you to know how early damage can be caught. They want you sick and dependent.
November 5, 2025 AT 11:20 AM
I used to ignore fatigue. Now I know it's my liver whispering. I got my ALT checked last month. Normal. Felt like I just won the lottery. You don't know how lucky you are until you almost lost it.
November 5, 2025 AT 19:10 PM
The ontological crisis of pharmacological agency: we are not subjects of our own physiology, but vectors of metabolic entropy. The body as a site of pharmakon - both cure and poison - reveals the inherent paradox of modern therapeutics. We weaponize biochemistry against itself.
November 6, 2025 AT 21:17 PM
My mom was on isoniazid for TB. They did monthly liver tests. She didn't even know why. Now she's fine. But if they hadn't checked? She wouldn't be here. So if you're on meds, just do the damn bloodwork. It's not that hard.
November 7, 2025 AT 21:24 PM
Oh wow so the liver breaks down acetaminophen into poison? Shocking. Next you'll tell me water can drown you if you drink too much. Groundbreaking science.
November 9, 2025 AT 03:08 AM
You think this is about drugs? Nah. It's about the chip. They put it in your meds to slowly kill your organs so you'll need more pills. The 5G towers sync with your mitochondria. You think your fatigue is from the statin? It's the surveillance. Wake up.
November 10, 2025 AT 01:34 AM
I'm not a doctor but I know this: if you're tired, swollen, or just feel off - don't brush it off. Call your doc. Bring your list. You don't need to be an expert to save your life. Just be awake.
November 11, 2025 AT 12:15 PM
Americans think they're invincible. You take every pill under the sun then cry when your body breaks. This isn't a conspiracy. It's consequences. Stop blaming the system. Start taking responsibility.
November 12, 2025 AT 02:44 AM
I've been on PPIs for 12 years... and now I'm terrified. I read this article and my hands are shaking. I'm gonna stop tomorrow. But what if it's already too late? What if my brain is already rotting? I don't even know anymore.
November 13, 2025 AT 20:40 PM
I used to think kidney damage was for drug addicts or old people. Then my cousin, 38, got acute kidney failure from ibuprofen. He didn't even have a preexisting condition. Now he's on dialysis. Don't be that person. Get tested.
November 14, 2025 AT 08:50 AM
So we're supposed to be scared of every pill now? Next you'll tell me breathing is dangerous because oxygen causes free radicals. Chill. You're giving people anxiety so you can sell them supplements.
November 15, 2025 AT 14:05 PM
The data here is solid. But the real barrier isn't knowledge - it's access. Not everyone can afford monthly labs or a second opinion. We need policy change, not just individual vigilance.
November 16, 2025 AT 03:04 AM
I'm 62 and on 7 meds. I don't know half of what they do. But I do know this: I write them all down. I bring them to every appointment. I ask one question: 'Could this hurt me?' Sometimes the answer surprises me. And that's enough.
November 17, 2025 AT 11:01 AM
THEY WANT YOU WEAK. The FDA, the AMA, the pharma CEOs - they ALL profit off your organ failure. The microRNA test? It's been banned from Medicare because it's too accurate. They'd lose billions. You think your doctor's on your side? He gets paid per pill prescribed.
November 19, 2025 AT 03:44 AM
The clinical imperative for proactive biomonitoring in pharmacotherapy is unequivocally supported by contemporary evidence-based guidelines from KDIGO, AASLD, and ESC. Failure to implement routine surveillance constitutes a breach of the standard of care.