When you’re managing type 2 diabetes, finding a medication that lowers blood sugar without causing low blood sugar or weight gain feels like a win. That’s why SGLT2 inhibitors became so popular. Drugs like canagliflozin, dapagliflozin, and empagliflozin work by making your kidneys flush out extra sugar through urine. Sounds simple, right? But here’s the catch: that same sugar in your urine doesn’t just disappear-it feeds bacteria and yeast. And that’s where things can go wrong.
How SGLT2 Inhibitors Work (and Why They Cause Infections)
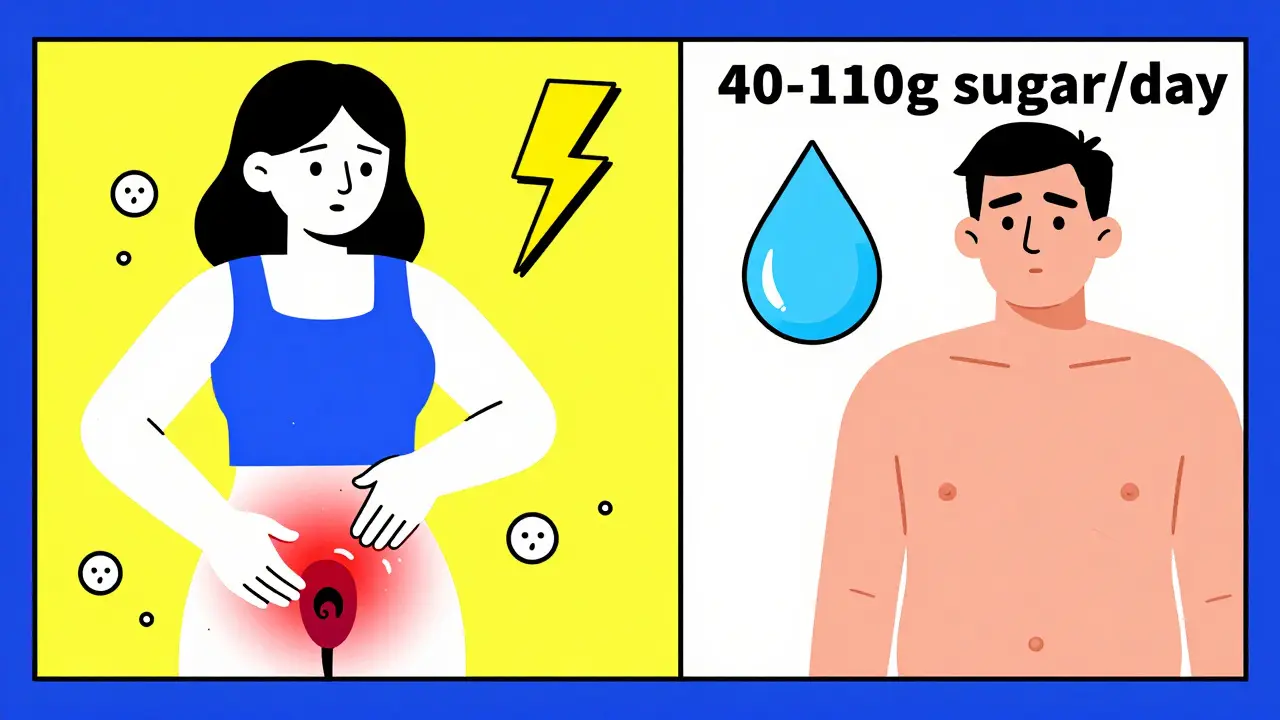
SGLT2 inhibitors block a protein in your kidneys that normally reabsorbs glucose. Instead of getting pulled back into your bloodstream, glucose gets dumped into your urine. On average, patients lose 40 to 110 grams of sugar daily through urine-roughly the equivalent of 10 to 25 teaspoons of sugar. That’s not just a number. It’s a feeding ground.
This sugar-rich environment doesn’t just attract bacteria. It creates the perfect breeding ground for Candida albicans, the fungus responsible for most yeast infections. The result? A spike in genital infections. Women report itching, redness, and thick white discharge. Men experience balanitis-swelling and discomfort under the foreskin. These aren’t rare side effects. Clinical trials show 3% to 5% of users develop genital yeast infections, compared to just 1% to 2% on placebo.
The Bigger Risk: Urinary Tract Infections and Beyond
Genital infections are bad enough, but they’re often mild and treatable. The real danger lies in what happens when those infections spread upward.
Studies show SGLT2 inhibitors increase the risk of urinary tract infections (UTIs) by nearly 80% compared to other diabetes drugs like DPP-4 inhibitors. That might sound small, but when you’re dealing with millions of patients, even a small percentage adds up. A 2022 meta-analysis found that for every 100 people taking an SGLT2 inhibitor, about 2 to 4 extra UTIs occur compared to those on other medications.
And some of those UTIs aren’t just uncomfortable-they’re life-threatening. The FDA reviewed data from 2013 to 2014 and found 19 cases of urosepsis, a blood infection originating in the urinary tract. Ten of those patients were on canagliflozin. Nine were on dapagliflozin. Four needed intensive care. Two required dialysis because their kidneys failed.
One case from the National Institutes of Health involved a 64-year-old woman who developed emphysematous pyelonephritis-a rare, gas-forming kidney infection-while taking dapagliflozin. She needed surgery. Eleven months later, after restarting the drug, she got another infection. This time, it was a perinephric abscess. She didn’t have a history of UTIs before starting the medication. That’s the pattern: no prior issues, then suddenly, a severe infection.
Who’s Most at Risk?
Not everyone on SGLT2 inhibitors gets infected. But some people are far more vulnerable.
- Women are more likely to get genital yeast infections than men, simply because of anatomy.
- People over 65 have weaker immune responses and often have other health issues that make infections harder to fight.
- Those with a history of UTIs or yeast infections are at much higher risk of recurrence.
- People with poor hygiene or limited access to clean water can’t flush out the sugar effectively.
- Those with kidney problems (eGFR below 60) are more likely to have concentrated sugar in their urine, increasing infection risk.
A 2024 study in Diabetes Care created a simple 5-point risk score: age over 65, female sex, HbA1c above 8.5%, prior UTI history, and low kidney function. If you score 3 or more points, your risk of a serious infection jumps to over 15%-that’s 1 in 7 people.
What About Fournier’s Gangrene?
It’s rare. But it’s terrifying.
Fournier’s gangrene is a fast-spreading, necrotizing infection of the genitals and perineum. It kills tissue. It spreads quickly. It can kill you if not caught early. The European Medicines Agency added a warning about it in 2016. Since then, fewer than 100 cases have been reported worldwide among millions of users. But every single case was linked to SGLT2 inhibitors.
One patient described waking up with swelling and fever, thinking it was a bad UTI. By the time he got to the hospital, the infection had spread to his abdomen. He needed multiple surgeries and months of recovery. He didn’t know the drug could cause this. He wasn’t warned.
How Do Doctors Decide Who Gets These Drugs?
SGLT2 inhibitors aren’t being pulled off the market. Why? Because they save lives.
In the EMPA-REG OUTCOME trial, empagliflozin reduced the risk of heart-related death by 38% in patients with heart disease. In the CANVAS trial, canagliflozin lowered heart attack and stroke risk by 14%. These drugs also slow kidney decline in people with diabetic kidney disease.
So doctors don’t avoid them-they choose carefully. The American Diabetes Association recommends SGLT2 inhibitors as a second-line option after metformin, but only if you have heart disease, heart failure, or kidney disease. If you’ve had recurrent UTIs or yeast infections, they’ll likely skip it and go with a GLP-1 agonist or DPP-4 inhibitor instead.
Doctors now screen before prescribing. They ask: “Have you ever had a yeast infection?” “Any UTIs in the last year?” “Do you have trouble cleaning your genital area?” If the answer is yes, they look at alternatives.
What Should You Do If You’re Already on an SGLT2 Inhibitor?
If you’re taking one of these drugs and feel fine, don’t panic. But stay alert.
- Watch for symptoms: Itching, burning, redness, swelling in the genital area. Pain when urinating. Cloudy or foul-smelling urine. Fever above 100.4°F. Back pain. Nausea. These aren’t normal.
- Hydrate more: Drink extra water-aim for at least 2 liters a day. It flushes sugar out faster and dilutes the urine.
- Practice good hygiene: Wash daily with mild soap. Dry thoroughly. Avoid tight clothing. Change underwear daily.
- Don’t ignore symptoms: If you think you have an infection, don’t wait. Call your doctor. Delaying treatment can turn a simple yeast infection into sepsis.
- Consider cranberry: A 2023 FDA safety update noted that cranberry supplements may reduce UTI risk by nearly 30% in SGLT2 users. It’s not a cure, but it’s a low-risk addition.

What If You’ve Had an Infection Already?
If you’ve had one serious infection-like a kidney infection or Fournier’s gangrene-most doctors will advise you to stop the SGLT2 inhibitor permanently. The risk of recurrence is high. One patient in a NIH case report had two life-threatening infections after restarting the drug. That’s not luck-it’s biology.
Swedish data shows that nearly 24% of patients quit SGLT2 inhibitors within two years because of genital or urinary side effects. That’s more than double the rate of people stopping DPP-4 inhibitors for similar reasons.
It’s not that these drugs are dangerous. It’s that they’re powerful-and they come with trade-offs. For some, the heart and kidney protection is worth the risk. For others, the infections are too much to handle.
Are There Safer Alternatives?
Yes. And they’re often just as effective.
- GLP-1 receptor agonists (like semaglutide or liraglutide) lower blood sugar, promote weight loss, and reduce heart risk-without increasing yeast or UTI risk.
- DPP-4 inhibitors (like sitagliptin or linagliptin) have almost no infection risk and are well tolerated.
- Metformin remains first-line for most people. It’s cheap, safe, and doesn’t cause infections.
The choice isn’t about which drug is “best.” It’s about which one fits your body, your history, and your priorities.
Bottom Line: Knowledge Is Protection
SGLT2 inhibitors are not bad drugs. They’re powerful tools that help people live longer, healthier lives. But they’re not for everyone. The same mechanism that lowers blood sugar also creates a risk for serious infections. That’s not a flaw in the drug-it’s a consequence of how it works.
If you’re on one, know the signs. If you’re considering one, ask the right questions. Talk to your doctor about your history of infections, your hygiene habits, your kidney function, and your overall health. Don’t assume it’s safe just because it’s prescribed. Don’t assume it’s dangerous just because it has warnings.
Diabetes care isn’t about picking the most popular drug. It’s about picking the right one-for you.



January 4, 2026 AT 04:02 AM
SGLT2 inhibitors are a classic trade-off: great for heart and kidneys, but your private parts pay the price. I’ve seen patients go from asymptomatic to ER visits in weeks. Hydration and hygiene aren’t optional-they’re part of the treatment plan now.
January 4, 2026 AT 12:06 PM
Big Pharma knew this was coming. They buried the data on yeast infections for years. Now they’re selling you ‘cranberry supplements’ like it’s a magic fix. Wake up. They don’t care if you lose a kidney-they care about your insurance premiums.
January 4, 2026 AT 20:29 PM
So let me get this straight-we’re giving people drugs that turn their pee into a sugar buffet… and then telling them to drink more water? Brilliant. Next up: ‘Eat more kale to offset your IV drip of insulin.’
January 5, 2026 AT 21:45 PM
It’s not just about the sugar in urine-it’s about the microbiome disruption. The bladder isn’t just a reservoir; it’s an ecosystem. Flooding it with glucose is like dumping honey into a beehive and wondering why the wasps show up.
And yes, cranberry helps-but not because it ‘kills bacteria.’ It prevents adhesion. Subtle, but critical.
January 6, 2026 AT 23:01 PM
If you’re on one of these meds, please don’t wait until you’re feverish to call your doctor. I’ve had patients ignore itching for weeks… then end up in the ICU. You’re not being dramatic-you’re being smart.
Keep a journal: note symptoms, water intake, when you last changed underwear. Small habits save lives.
January 7, 2026 AT 18:26 PM
For those concerned about alternatives: GLP-1 agonists like semaglutide have comparable cardiovascular benefits, with lower infection risk. They’re more expensive, yes-but so is a hospital stay for urosepsis.
Cost-benefit analysis isn’t just about the pill. It’s about the ICU bill.
January 9, 2026 AT 16:18 PM
Let me ask you: if this drug causes yeast infections, why isn’t it classified as a fungal culture medium? And why do regulatory bodies still allow it? Is it because the patients who suffer are statistically insignificant? Or is it because the shareholders aren’t?
Also, why is ‘drink more water’ the primary recommendation? Why not ‘stop taking the drug’? Hypocrisy is the new standard.
January 11, 2026 AT 02:30 AM
In Nigeria, we don’t have access to fancy drugs like this-but we do know one thing: if your pee tastes sweet, something’s wrong. Not just for diabetes-your whole body is screaming.
My cousin took this med, got a yeast infection, and thought it was ‘just a rash.’ He didn’t go to the clinic until he couldn’t walk. Now he’s on metformin. Simple. Safe. Effective.
Don’t let fancy science make you forget common sense.
January 12, 2026 AT 21:37 PM
As an Indian man who’s been on dapagliflozin for 2 years-yes, I got a mild yeast infection. No big deal. I used clotrimazole, drank coconut water, and kept it dry. Problem solved.
But I also had a heart attack last year. This drug kept me alive. So I’ll take the itch over the ICU any day.
It’s not perfect-but it’s better than the alternative.
January 13, 2026 AT 20:51 PM
We’ve turned medicine into a math problem: risk of death from heart disease vs. risk of itching. But what about the soul? The dignity? The quiet shame of having to explain to your partner why you can’t sleep because your skin is on fire?
These drugs don’t just alter biology-they alter intimacy. And no one talks about that.
January 14, 2026 AT 13:48 PM
My uncle took one of these. Got a UTI. Then another. Then a kidney infection. He’s fine now-but he says he’d rather have high sugar than high drama. I get it.
These meds aren’t evil. They’re just… loud. And sometimes, silence is better.
January 15, 2026 AT 03:32 AM
Why are we even talking about this? If you’re too weak to handle a little yeast, maybe you shouldn’t be on a diabetes drug at all. Get your life together. Stop eating sugar. Exercise. Drink water. Stop blaming Big Pharma.
January 16, 2026 AT 19:15 PM
It’s not the drug’s fault. It’s not the patient’s fault. It’s the system’s fault. We treat diabetes like a number to fix, not a whole body to care for.
We prescribe a pill and say ‘drink water’ like it’s a magic bullet. But we don’t provide nutrition counseling. We don’t check access to clean bathrooms. We don’t ask if they can afford antifungal cream.
The infection isn’t in the urine. It’s in the care model.
January 17, 2026 AT 05:20 AM
I’ve been on canagliflozin for 18 months. No infections. I drink 3 liters a day. I shower after every meal. I wear cotton. I don’t use scented soap.
So don’t tell me it’s inevitable. It’s not the drug. It’s the laziness.
January 17, 2026 AT 20:15 PM
People like you think you’re so smart because you read a medical journal. But you’re just enabling a culture of weakness. If your body can’t handle a little sugar in your pee, maybe you shouldn’t be alive.
My grandpa had diabetes in the 80s. He didn’t have fancy drugs. He walked 5 miles a day. He ate rice and beans. He lived to 92.
You’re not sick. You’re spoiled.
January 18, 2026 AT 14:21 PM
According to the 2024 Diabetes Care risk score, I’m a 5/5: female, 68, HbA1c 9.1%, prior UTI, eGFR 52. My risk is 17%. My doctor switched me to semaglutide. No more itching. No more fear. Just better control. The data doesn’t lie. The risk score works.
January 19, 2026 AT 17:04 PM
so i started taking dapagliflozin and like… i think i got a yeast infection?? but im not sure bc my boyfriend says its just my period?? and now im scared to go to the dr bc theyll judge me??
January 20, 2026 AT 16:49 PM
As a physician in rural India, I see patients who have never heard of SGLT2 inhibitors. They take whatever is cheapest. Many develop infections. We treat them with local herbs and hygiene education. The real issue is not the drug-it is the absence of context.
Medicine without cultural understanding is not medicine. It is a gamble.
January 21, 2026 AT 13:50 PM
Let’s be honest: if this drug caused 10x more infections, it would’ve been pulled. The fact that it’s still on the market means the risk is acceptable. Your discomfort is not a crisis. Your life is.