Acid-Reducing Medication Interaction Checker
Check Your Medication Safety
Enter the medications you're taking and select your acid reducer to see potential interactions.
When you take a pill for heartburn, you might not think it could mess with your other meds. But that’s exactly what happens with acid-reducing drugs like PPIs (proton pump inhibitors) and H2 blockers. These medications are everywhere - millions of people use them daily for acid reflux, ulcers, or even just occasional discomfort. But behind the scenes, they’re quietly changing how your body absorbs other drugs. And in some cases, that change can be dangerous.
How Acid-Reducing Drugs Work
Your stomach normally has a very low pH - between 1.0 and 3.5 when you’re fasting. That’s about as acidic as lemon juice. This acidity isn’t just for digestion; it’s also critical for how certain drugs dissolve and get absorbed. Acid-reducing medications like omeprazole (Prilosec), esomeprazole (Nexium), or famotidine (Pepcid) raise that pH, sometimes all the way to 4.0 or even 6.0. That sounds harmless, even helpful. But for many drugs, it’s a game-changer.
PPIs work by shutting down the proton pumps in stomach cells that produce acid. They’re powerful and long-lasting - often keeping your stomach less acidic for 14 to 18 hours a day. H2 blockers like ranitidine or cimetidine block histamine signals to reduce acid, but they’re not as strong or long-lasting. The difference matters. PPIs cause bigger, longer pH shifts, which means they’re far more likely to interfere with other medications.
The Science Behind the Interference
Most drugs don’t just float through your stomach - they need to dissolve first. Whether they dissolve depends on their chemical structure, especially their pKa - a number that tells you how a drug behaves in different pH levels. About 70% of oral medications are weak bases, meaning they dissolve better in acid. Think of them like salt: salt dissolves in water, but not in oil. In a low-pH (acidic) stomach, these drugs dissolve easily. But when acid is suppressed, they stay locked up, undissolved, and can’t be absorbed.
Take atazanavir, a drug used to treat HIV. It’s a weak base with a pKa around 5.2. In a normal acidic stomach, it dissolves fine. But when taken with a PPI, its absorption drops by 74% to 95%. That’s not a small drop - it’s enough to let the virus come back. One patient on Reddit described their viral load jumping from undetectable to over 12,000 copies/mL after starting omeprazole. Their infectious disease doctor confirmed: classic interaction.
Dasatinib, used for chronic myeloid leukemia, drops 60% in absorption with PPIs. Ketoconazole, an antifungal, becomes almost useless. Even blood pressure meds like nilotinib can be affected, though less dramatically. The FDA estimates that 25% to 50% of the top 200 prescribed drugs in the U.S. are at risk. That’s hundreds of millions of prescriptions each year.
What About Acidic Drugs?
You might think if bases are affected, acids might be helped. That’s partly true. Weakly acidic drugs like aspirin (pKa 3.5) dissolve better in higher pH environments. But here’s the catch: most absorption happens in the small intestine, not the stomach. The stomach’s job is mostly to break things down. The small intestine has 200 to 300 square meters of surface area - way more than the stomach’s 1 to 2 square meters. So even if a drug dissolves better in the stomach, it’s not where most of it gets into your bloodstream.
That’s why acidic drugs rarely show big clinical changes. For example, dasiglucagon, used for low blood sugar, only sees a 15% to 20% increase in absorption with ARAs - not enough to require a dose change. The real danger lies with weak bases, especially those with narrow therapeutic windows. That means the difference between a dose that works and one that fails or causes toxicity is tiny.

PPIs vs. H2 Blockers: Which Is Worse?
Not all acid-reducers are equal. A 2024 study in JAMA Network Open found PPIs reduce absorption of pH-dependent drugs by 40% to 80%. H2 blockers? Only 20% to 40%. Why? Because PPIs are stronger and longer-lasting. One dose of omeprazole can suppress acid for over half a day. H2 blockers wear off in 8 to 12 hours.
Also, formulation matters. Immediate-release pills dissolve quickly in the stomach, so they’re more vulnerable. Extended-release versions are designed to release slowly, often bypassing the stomach’s pH changes. Enteric-coated pills - meant to dissolve only in the intestine - can backfire. If stomach acid is too low, they may dissolve too early, in the stomach, and get destroyed before they even get to the right spot.
Real-World Consequences
This isn’t theoretical. A 2023 study of over 12,500 patients found those taking dasatinib with a PPI had 37% higher rates of treatment failure. The FDA’s adverse event database recorded over 1,200 reports of drug interactions between 2020 and 2023. The top three offenders? Atazanavir, dasatinib, and ketoconazole.
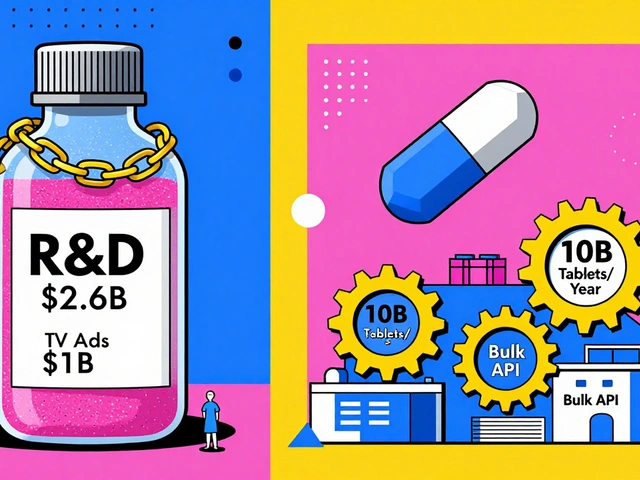
And it’s not just prescription drugs. Over-the-counter PPIs are sold in bottles with no warning labels. Many people take them daily for years, thinking they’re safe. The CDC says 15% of adults in developed countries use ARAs chronically - often without a clear medical reason. The American College of Gastroenterology says 30% to 50% of long-term PPI users don’t actually need them. That’s millions of people at risk for hidden, serious drug interactions.
How to Protect Yourself
If you’re on a medication that might be affected, here’s what to do:
- Know your drugs. If you’re taking a drug for HIV, cancer, or fungal infections - especially if it’s taken daily - ask your pharmacist or doctor if it’s sensitive to stomach pH.
- Ask about alternatives. If you need acid relief but take atazanavir or dasatinib, antacids like Tums or Maalox might be safer - if taken 2 to 4 hours apart. But they only last a few hours, so they’re not ideal for long-term use.
- Time your doses. If you must take both, space them out. Take the affected drug at least 2 hours before the PPI. This doesn’t fix everything, but studies show it can cut the interaction by 30% to 40%.
- Check your pill type. Is it immediate-release? Enteric-coated? Extended-release? These details matter. Don’t assume all versions of a drug behave the same.
- Use a pharmacist. A 2023 study showed pharmacist-led reviews cut inappropriate ARA co-prescribing by 62% in Medicare patients. Pharmacists see all your meds. They’re trained to spot these issues.
What’s Being Done
The FDA now requires drug labels to include specific warnings about ARA interactions. Between 2020 and 2023, 28 drug labels were updated - up from just 12 in the prior five years. New drugs in development are being designed to avoid pH dependence altogether. Thirty-seven percent of new molecular entities now use delivery systems that bypass stomach pH changes.
Electronic health records now alert doctors when a PPI is prescribed alongside a high-risk drug. Epic Systems reports 78% of clinicians follow those alerts. AI tools are also emerging. Google Health’s prototype can predict these interactions with 89% accuracy.
The bigger picture? Deprescribing. Many people take PPIs long after they need them. The American Gastroenterological Association aims to reduce inappropriate ARA use by 25% by 2027. That could prevent 5,000 to 7,000 cases of treatment failure every year.
Final Thoughts
Acid-reducing drugs aren’t bad. They save lives. But they’re not harmless either. When used without need, or without checking for interactions, they can silently undermine other treatments. The key is awareness. If you’re on a medication that’s critical to your health - especially for HIV, cancer, or serious infections - don’t assume your heartburn pill is safe. Talk to your doctor. Ask your pharmacist. And if you’ve been taking a PPI for years, it might be time to ask whether you still need it.
Can acid-reducing medications make my other drugs stop working?
Yes, especially if you’re taking weakly basic drugs like atazanavir, dasatinib, or ketoconazole. These drugs need stomach acid to dissolve properly. When PPIs or H2 blockers raise stomach pH, they can reduce absorption by up to 95%, leading to treatment failure. This is well-documented in clinical studies and FDA reports.
Which is riskier: PPIs or H2 blockers?
PPIs are significantly riskier. They suppress acid more deeply and for longer - often 14 to 18 hours a day - compared to H2 blockers, which last 8 to 12 hours. Studies show PPIs reduce absorption of pH-sensitive drugs by 40-80%, while H2 blockers cause 20-40% reductions. If you must use an acid reducer and take a high-risk drug, H2 blockers are the safer choice - but even then, timing matters.
I take omeprazole for heartburn. Should I stop it?
Don’t stop it without talking to your doctor. But do ask whether you still need it. About half of long-term PPI users don’t have a clear medical reason for taking it. The American College of Gastroenterology recommends reassessing PPI use every 6 to 12 months. If you’re taking it just for occasional discomfort, lifestyle changes or antacids might be enough.
Can I just take my meds at different times to avoid the interaction?
Spacing them out helps, but it’s not a full fix. Taking the affected drug 2 hours before the PPI can reduce the interaction by 30-40%. For example, with dasatinib, studies show this approach restores effectiveness in 85% of cases. But it doesn’t eliminate the risk entirely. For drugs like atazanavir, even this doesn’t work well - complete avoidance is recommended.
Are over-the-counter PPIs safer than prescription ones?
No. OTC PPIs like Prilosec OTC or Nexium 24HR contain the same active ingredients and work the same way as prescription versions. The difference is only in dosage and how long you’re supposed to take them. Many people use OTC PPIs daily for months or years, unaware of the risks. They’re not safer - just more accessible.
How do I know if my drug is affected?
Check the drug label - the FDA now requires interaction warnings. Common high-risk drugs include atazanavir, dasatinib, ketoconazole, mycophenolate, erlotinib, and certain antibiotics like ciprofloxacin. If you’re unsure, ask your pharmacist. They can look up your medications and flag any potential issues. You can also search for your drug + "PPI interaction" online - reputable sources like the FDA or Micromedex have this info.

February 13, 2026 AT 15:26 PM
I get that PPIs can mess with meds, but honestly? I’ve been on omeprazole for 8 years and my blood pressure is better than ever. My doc says my atazanavir levels are stable. Maybe it’s not as universal as they make it sound? People act like every single person is one pill away from dying. I’m just saying - your mileage may vary. 🤷♀️