Getting the right dose of liquid medicine isn’t just about following the label-it’s about staying safe. Every year, over a million people in the U.S. are injured because someone gave the wrong amount of liquid medication. Most of these mistakes happen because people misread the label or use the wrong tool to measure. It doesn’t matter if you’re giving medicine to a baby, a child, or an older adult. If you don’t know how to read the numbers and units on the bottle, you’re at risk.
Why Milliliters (mL) Are the Only Unit You Should Trust
Look at the label. Do you see mL? That’s good. If you see teaspoons (tsp) or tablespoons (tbsp), that’s a red flag. Even though some older labels still use them, the FDA and the National Council for Prescription Drug Programs (NCPDP) have been pushing for milliliters only since 2015. Why? Because a kitchen teaspoon can hold anywhere from 2.5 to 7.5 milliliters. A tablespoon? It might be 5 mL or it might be 20 mL. That’s a 300% difference. One wrong spoon, and you could be giving your child three times the dose they need.
Pharmacies in the U.S. are supposed to use mL on all new liquid prescriptions. By 2021, 68% of pharmacies had fully adopted this rule. Major chains like CVS, Walgreens, and Rite Aid are nearly 100% compliant. But smaller, independent pharmacies? Only about 58% are fully on board. If you get a label that says “take 1 tsp,” ask the pharmacist to rewrite it in mL. They’re required to do it.
Understanding Concentration: What Does ‘125 mg/5 mL’ Mean?
The dose isn’t just the number of milliliters. You also need to know how much medicine is in each milliliter. That’s called the concentration. It’s written like this: 125 mg/5 mL. This means every 5 mL of liquid contains 125 milligrams of the active drug.
Here’s where people get confused. They see “500 mL” on the bottle and think that’s the dose. It’s not. That’s the total amount of liquid in the whole bottle. The dose is what the doctor told you to give at one time. For example, if the label says “Take 10 mL twice daily,” and the concentration is “125 mg/5 mL,” then you’re giving 250 mg each time (because 10 mL is two 5 mL portions, and 125 mg × 2 = 250 mg).
Always check both the dose amount (e.g., 10 mL) and the concentration (e.g., 125 mg/5 mL). If you’re unsure, ask the pharmacist to explain it out loud. Don’t just nod and leave.
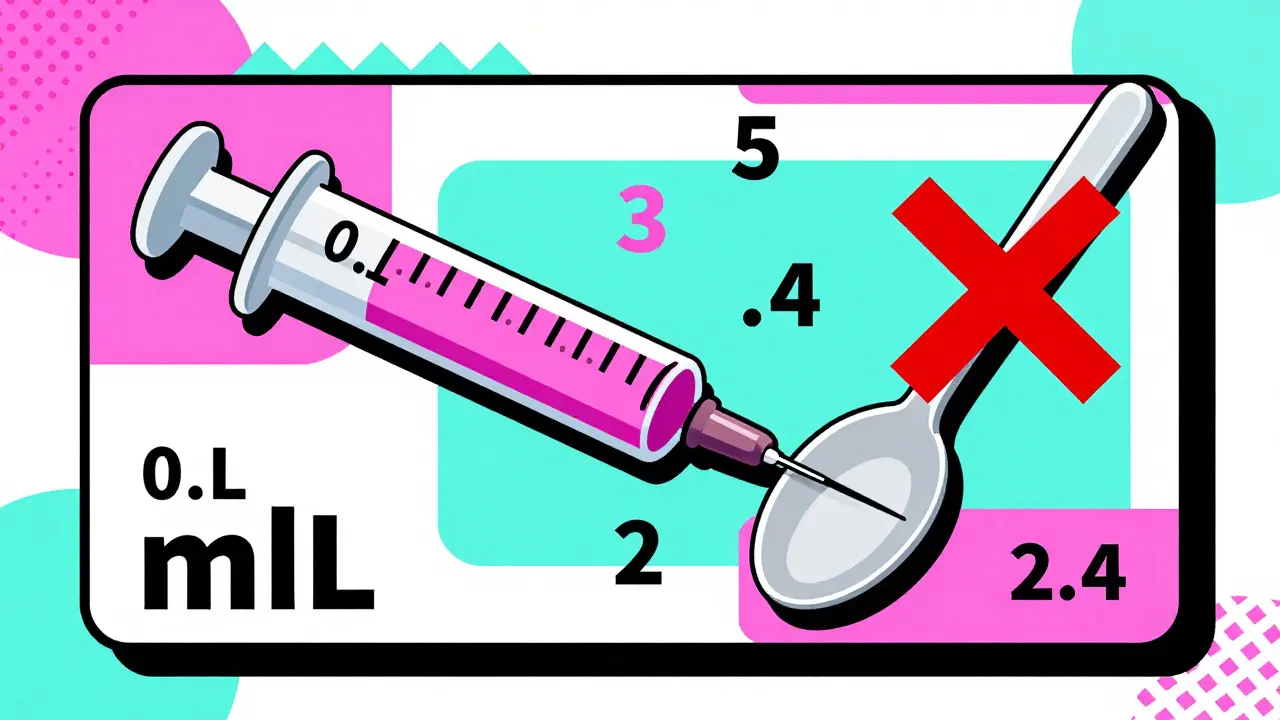
Decimal Points and Zeros: Small Details, Big Risks
Look closely at the numbers. A tiny mistake can be deadly.
- Always write and read doses with a leading zero: 0.5 mL, never .5 mL. Without the zero, someone might misread it as 5 mL-ten times too much.
- Never use trailing zeros: 5 mL, never 5.0 mL. That extra decimal can make someone think the dose is more precise than it is, leading to dangerous over-measuring.
A Johns Hopkins study in 2018 found that using these formatting rules cut 10-fold dosing errors by 47%. That’s nearly half the mistakes avoided just by writing numbers correctly.
Also, make sure there’s space between the number and the unit: 5 mL, not 5mL. That tiny space helps your brain separate the number from the unit so you don’t accidentally read “5mL” as “50 mL” or something else.

Use Only the Measuring Tool That Comes With the Medicine
Never use a kitchen spoon, a shot glass, or a regular medicine cup from last time. Each liquid medication comes with its own measuring device-usually a syringe, a cup, or a dropper. That device is made to match the exact dose on the label.
For example, if your label says “Give 2.4 mL,” the syringe will have lines for 2.0 mL and 2.5 mL. You’ll fill it to the line closest to 2.4 mL. A kitchen teaspoon can’t do that. Even a plastic dosing cup from a different medicine might not have the right markings.
Studies show that parents who use the tool that comes with the medicine make 52% fewer mistakes than those who use household spoons. And if the tool is missing? Call the pharmacy. They’ll give you a new one for free. Don’t improvise.
What to Do If the Label Is Confusing or Missing Info
Some labels still have problems. Maybe the concentration is too small to read. Maybe the dose isn’t clear. Maybe there’s no measuring tool. Here’s what to do:
- Check the expiration date. If it’s expired, don’t use it. Throw it out and get a new prescription.
- Look for the total volume. Most liquid prescriptions come in 118 mL or 237 mL bottles. If you don’t see that, ask.
- If the concentration is printed in tiny font, ask the pharmacist to write the dose on a sticky note: “Give 4 mL every 6 hours.”
- If the label says “as needed” or “up to 2 doses,” make sure you know the maximum number of doses per day. Don’t guess.
Pharmacists are trained to catch these issues. But they can’t help if you don’t ask. Take 30 seconds before you leave the pharmacy to confirm: “Can you show me how much to give?”
Teach-Back: The Simple Trick That Prevents 63% of Errors
One of the most powerful tools in medicine isn’t a device or a rule-it’s a conversation. Ask the pharmacist: “Can you show me how to give this dose?” Then, after they show you, say: “Okay, I’ll do it now.”
That’s called the “teach-back” method. You’re not just listening-you’re demonstrating. And it works. According to the Agency for Healthcare Research and Quality (AHRQ), using teach-back reduces dosing errors by 63%.
It’s especially important with children. If you’re giving medicine to a baby or toddler, don’t just rely on memory. Practice with the syringe in front of the pharmacist. Make sure you know how to draw up the exact amount without air bubbles. If you’re not confident, ask again. No one will think less of you.
What About Smart Labels and QR Codes?
The future of medication safety is already here. Some pharmacies, like Amazon Pharmacy and McKesson’s Medly, are putting QR codes on labels. Scan it with your phone, and you’ll see a short video showing exactly how to measure the dose.
Early results show these smart labels reduce error-related calls by 28%. The FDA is pushing for pictograms on all liquid labels by 2025-simple icons showing a syringe filling to a line, or a child taking medicine. These visual cues help people who struggle with reading or have low health literacy.
Right now, only a few pharmacies offer this. But it’s coming fast. If your pharmacy doesn’t have it yet, ask if they plan to add it. Consumer demand is driving change.
Final Checklist Before You Give the Dose
Before you open the bottle, run through this quick list:
- Is the dose in mL? If not, ask for a corrected label.
- What’s the concentration? (e.g., 160 mg/5 mL)
- How much am I giving? (e.g., 5 mL)
- Do I have the right tool? (Use only the one that came with the medicine)
- Is the number written correctly? (0.5 mL, not .5 mL; 5 mL, not 5.0 mL)
- Did I check the expiration date?
- Did I demonstrate it back to the pharmacist? (Teach-back)
If you answer yes to all six, you’re doing better than 70% of people who give liquid medicine. That’s not luck. That’s safety.
Why This Matters More Than You Think
Liquid medicines are given to kids more than any other group. In fact, 75% of all liquid prescriptions are for children under 12. And kids are more sensitive to overdoses. A little too much can mean drowsiness, breathing trouble, or even seizures.
But it’s not just kids. Older adults on multiple medications often mix up their bottles. People with vision problems or low literacy struggle to read tiny print. That’s why standardization matters. It’s not about rules-it’s about preventing harm.
Every time you read a label correctly, you’re not just following instructions. You’re protecting someone you love.
Can I use a kitchen teaspoon if I don’t have a measuring cup?
No. A kitchen teaspoon can hold anywhere from 2.5 to 7.5 milliliters, which is far too inconsistent for safe dosing. Even if you think your spoon holds exactly 5 mL, you can’t be sure. Always use the measuring tool that came with the medicine. If you lost it, call the pharmacy-they’ll give you a new one for free.
Why do some labels say ‘5.0 mL’ instead of ‘5 mL’?
That’s a mistake. The FDA and NCPDP guidelines say never to use trailing zeros after a whole number. ‘5.0 mL’ can make someone think the dose is more precise than it is, leading to dangerous over-measuring. Always trust the version that says ‘5 mL.’ If you see ‘5.0 mL,’ ask the pharmacist to confirm the correct dose.
What if the label says ‘take 0.8 mL’? How do I measure that?
You need a syringe that measures down to 0.1 mL. Most pediatric liquid medicines come with a 1 mL or 5 mL syringe that has fine lines for small doses. Fill the syringe slowly and look at the line closest to 0.8 mL. If your syringe doesn’t have those lines, return to the pharmacy and ask for a different one. Never guess or round up to 1 mL unless the pharmacist tells you it’s safe.
My child’s medicine label says ‘120 mg/5 mL’ and the dose is ‘10 mL.’ How much medicine am I giving?
You’re giving 240 mg. The concentration is 120 mg per 5 mL. Since you’re giving 10 mL, that’s two times 5 mL. So, 120 mg × 2 = 240 mg. Always multiply the concentration by the number of 5 mL portions in your dose. If you’re unsure, ask the pharmacist to break it down for you.
Can I trust the dose markings on the medicine cup that came with the bottle?
Yes-if it’s the one that came with this specific bottle. Some cups have both mL and tsp markings. Always use the mL side. If the cup has a line for your dose, fill to that line. Don’t use a different cup from another medicine, even if it looks similar. Each cup is calibrated for its own medication’s concentration.
What should I do if I accidentally give the wrong dose?
Call your pharmacist or poison control immediately. Don’t wait for symptoms. In the U.S., call Poison Control at 1-800-222-1222. They can tell you if it’s dangerous and what to watch for. Keep the bottle and the measuring tool with you when you call. The more details you give, the better they can help.
December 28, 2025 AT 03:30 AM
mL only. no more tsp. i used a spoon once for my kid and almost panicked when the pharmacist caught it. free measuring cup next time, no excuses.
December 29, 2025 AT 04:36 AM
people still use kitchen spoons? bro. you're not cooking curry. this is medicine. one wrong spoon and your kid's in the ER. stop being lazy.
December 30, 2025 AT 19:19 PM
This isn't just about numbers-it's about trust. The way we handle medicine reflects how much we care. That tiny line on a syringe? That's love in milliliters. Don't guess. Don't wing it. Show up for them like the dose demands.
December 31, 2025 AT 00:12 AM
I find it deeply concerning that the FDA has to spell this out like we're children. We live in a society where people can't distinguish between 5 mL and 5.0 mL, yet they're entrusted with the lives of infants. The failure of public health literacy is not an accident-it is a systemic collapse.
December 31, 2025 AT 20:05 PM
I used to think I was careful-until I saw a mom at the pharmacy trying to use a soup spoon for her 8-month-old's antibiotics. I almost cried. Then I realized-this isn't about one mom. It's about a culture that treats medicine like a suggestion. The fact that we still have to explain that 0.5 mL isn't 5 mL... that's not incompetence. That's neglect. And it's killing people. Every day. Quietly. Unnoticed. Until it's too late.
January 1, 2026 AT 15:05 PM
YES. YES. YES. I just started giving my daughter her meds and I used the syringe. I actually felt like a superhero. That little plastic tool? It’s a lifeline. And if you lose it? CALL THE PHARMACY. THEY’LL GIVE YOU A NEW ONE. NO EXCUSES.
January 1, 2026 AT 22:24 PM
I’ve worked in pharmacy for 17 years. I’ve seen parents cry because they gave 10 mL instead of 1.0 mL. I’ve seen kids in the ER because someone thought ‘5.0’ meant ‘more precise’ so they gave more. I’ve seen labels with no concentration printed. I’ve seen it all. And I’m telling you-this checklist? It’s not a suggestion. It’s your child’s last line of defense. Print it. Tape it to the fridge. Memorize it. Don’t let your love become their poison.
January 2, 2026 AT 06:10 AM
i read this while holding my niece’s medicine bottle. i had no idea about the 0.5 vs .5 thing. i always thought it was the same. now i feel a little ashamed but also grateful. thank you for writing this like you actually care.
January 2, 2026 AT 18:24 PM
my cousin gave his kid 5ml of tylenol using a spoon and the kid got sick. we all thought it was fine until the hospital called. now he only uses the syringe. dumb mistake. easy fix.
January 3, 2026 AT 01:42 AM
i used to think the little cup was fine but then i realized it had tsp and ml and i was using tsp by accident. now i only use the syringe and i write the dose on a sticky note. its so much easier. thanks for reminding me!
January 3, 2026 AT 22:30 PM
this is so basic why is this even a post? if you can't read a label you shouldn't be parenting. also why are we letting pharmacies get away with printing concentration in 4pt font? this is a crime against humanity.
January 5, 2026 AT 17:50 PM
The epistemological crisis of pharmaceutical literacy is not merely a matter of measurement-it is a metaphysical failure of the modern subject to engage with the materiality of care. The milliliter, as a unit, is not neutral; it is a signifier of societal decay. To use a teaspoon is to reject the ontological responsibility of parenthood. The trailing zero? A Cartesian illusion of precision masking existential negligence.
January 7, 2026 AT 15:14 PM
In India, we often use teaspoons because syringes aren’t always available. But I’ve started asking for them anyway. Pharmacists here are usually happy to help. It’s not about wealth-it’s about awareness. And this post? It’s a quiet revolution.
January 9, 2026 AT 05:56 AM
Just use the syringe. No exceptions.