Kava and Sedative Medications: What You Need to Know About Liver and Sedation Risks
If you're taking medication for anxiety, sleep, or pain - like benzodiazepines, sleep aids, or even antidepressants - and you're also using kava, you're playing with fire. Not because kava is inherently dangerous, but because it doesn't play well with the drugs millions of people take every day. The combination can make you dangerously sleepy, blur your thinking, and in rare but real cases, wreck your liver.
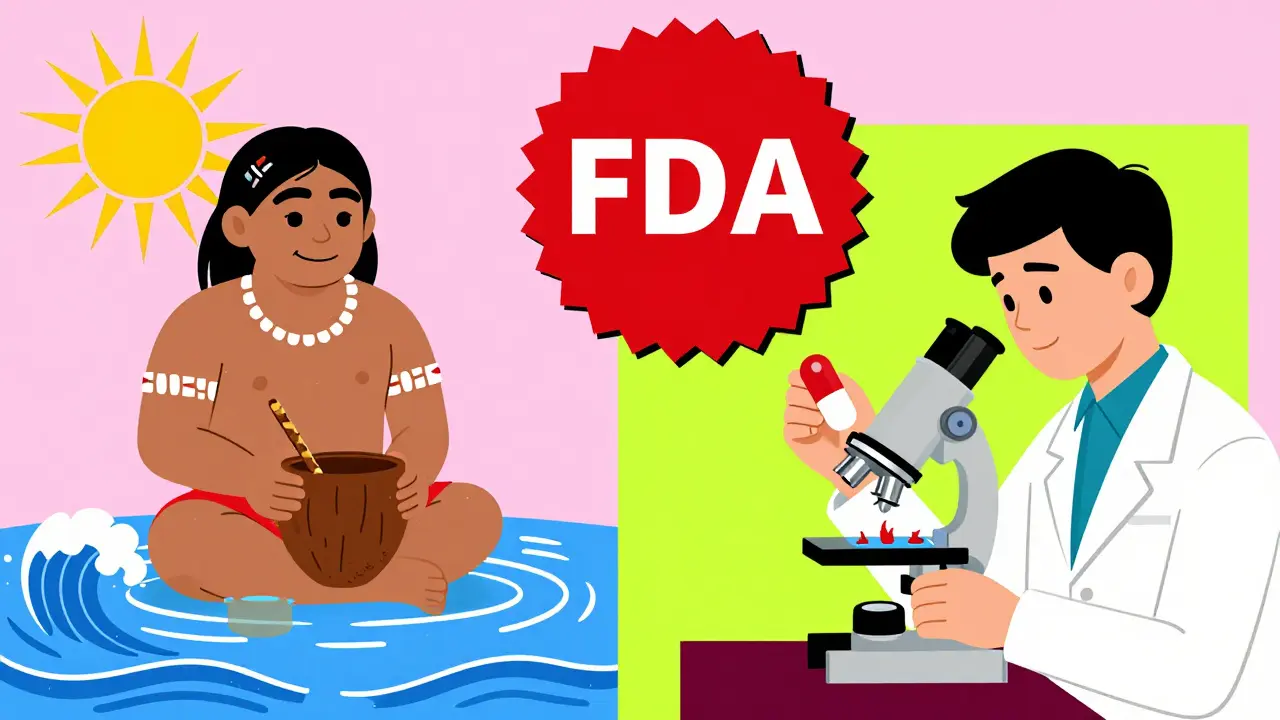
Kava, made from the roots of the Piper methysticum plant, has been used for centuries in Pacific Island cultures for calming ceremonies. Today, it’s sold in capsules, teas, and tinctures in the U.S. as a natural remedy for stress and insomnia. But unlike prescription drugs, it’s not tightly regulated. One bottle might have 70 mg of active compounds. Another might have 300 mg. That’s a huge difference - and it’s why some people get sick while others don’t.
How Kava Works - and Why It’s Risky With Medications
Kava’s effects come from a group of chemicals called kavalactones. The main ones - kavain, dihydrokavain, methysticin, and yangonin - cross the blood-brain barrier in under 15 minutes. They calm the nervous system by slowing down brain signals, similar to how alcohol or Xanax works. That’s why people feel relaxed, sometimes even a little floaty, within 30 to 90 minutes after taking it.
But here’s the hidden problem: kava also interferes with your liver’s ability to break down other drugs. It blocks key enzymes - CYP2D6, CYP2C9, and CYP3A4 - that your body uses to process sedatives like alprazolam (Xanax), diazepam (Valium), lorazepam (Ativan), and even some painkillers and antidepressants. When those enzymes are blocked, the medication builds up in your blood. A normal dose of Xanax might become too strong. That’s why some people end up so drowsy they can’t stand up, or worse, end up in the hospital.
A Sacramento County case study from 2023 showed two patients who developed severe liver damage after combining kava with prescription sedatives. One had ALT levels (a liver enzyme) skyrocket to 2,840 U/L - normal is under 40. The other had a dangerous blood clotting issue with an INR of 4.2. Both needed hospital care.
How Dangerous Is the Liver Damage?
The FDA issued a warning about kava and liver injury back in 2002. Since then, over 25 international cases have been reported, with some patients needing liver transplants. The numbers sound low - less than 1 in a million daily doses - but the problem isn’t frequency. It’s unpredictability.
One person might take kava for a year with no issues. Another might take it for six weeks and end up with hepatitis. There’s no way to know who’s at risk. And it’s not just about how much you take. It’s about what else you’re taking, your genetics, your liver health, and even how the kava was prepared.
Traditional Pacific Islanders make kava by grinding the root and mixing it with cold water. That method pulls out the calming kavalactones but leaves behind compounds linked to liver stress. Commercial supplements? Many are made with alcohol or acetone to extract more kavalactones - and those solvents pull out the bad stuff too. The World Health Organization found that water-based kava drinks have 9 times fewer adverse events than alcohol-extracted supplements.
That’s why Australia’s Therapeutic Goods Administration says the risk is low - but only if you stick to traditional water extracts and don’t go over 250 mg per day. If you’re using capsules from a random online store? You’re in the dark.

What Happens When Kava Meets Sedatives?
Combining kava with sedatives isn’t just risky - it’s a recipe for overdose. You don’t need to take a ton of either. Even a low dose of kava (70 mg) with a standard dose of lorazepam (0.5 mg) can cause extreme drowsiness, confusion, and loss of coordination.
Reddit users have shared dozens of stories. One wrote: “Took kava with my 0.5 mg lorazepam. Couldn’t stand for 8 hours. Speech was slurred. Felt like I was drunk but sober.” Another said they passed out after dinner and woke up hours later with no memory of the time in between.
WebMD rates kava’s interaction with benzodiazepines as “major.” Studies show kava can increase the blood levels of midazolam - a powerful sedative - by 27%. That’s not a small bump. That’s enough to push someone into respiratory depression, especially if they’re older or have other health issues.
And it’s not just prescription drugs. Alcohol? Even one drink with kava can double the sedation risk. Some users report blacking out after just one glass of wine and a kava capsule. That’s not a party trick. That’s a medical emergency waiting to happen.
Who Should Avoid Kava Completely?
If you’re on any of these, don’t take kava:
- Any benzodiazepine (Xanax, Valium, Ativan, Klonopin)
- Sleep medications (Ambien, Lunesta, zaleplon)
- Antidepressants like SSRIs or SNRIs (especially if they’re metabolized by CYP enzymes)
- Antipsychotics like haloperidol (risk of dangerous heart rhythm changes)
- Opioid painkillers (oxycodone, hydrocodone)
- Alcohol - even occasionally
- You have any history of liver disease - hepatitis, fatty liver, elevated liver enzymes
- You’re over 65 - your liver processes drugs slower
- You’re pregnant or breastfeeding
The CDC and American Association for the Study of Liver Diseases say: if you have liver problems, skip kava entirely. No exceptions.
What If You’re Already Taking Both?
If you’ve been mixing kava with your meds and feel fine, that doesn’t mean you’re safe. Liver damage often shows up silently - no pain, no symptoms - until it’s advanced.
Here’s what to do right now:
- Stop taking kava immediately.
- Don’t quit your prescription meds cold turkey - talk to your doctor first.
- Ask for a liver function test (ALT, AST, bilirubin, INR). Even if you feel okay, get baseline numbers.
- Bring all your supplements to your next appointment. Most doctors don’t ask about herbal products. You have to tell them.
Research from Sacramento County found that only 22% of patients with liver issues even mentioned they were taking kava - until their doctor asked directly. Don’t assume your doctor knows. They probably don’t.
Is There a Safe Way to Use Kava?
If you’re not on any sedatives and your liver is healthy, you *might* be able to use kava cautiously - but it’s not risk-free.
Here’s what the safest approach looks like:
- Only use water-extracted kava powder or tea - never alcohol-based tinctures or capsules
- Stick to 70-100 mg of kavalactones per day - no more
- Use it no more than 3-4 times a week, not daily
- Don’t use it for longer than 4 months straight
- Get liver tests every 6 weeks if you’re using it regularly
- Never mix with alcohol, sleep aids, or any CNS depressant
Even then, the science is unclear. The European Food Safety Authority says there’s no safe level for people taking medications. The FDA says it’s a warning, not a ban. Australia says it’s low risk - but only if you’re careful. There’s no universal green light.
What’s Happening Now? Regulatory Changes and Future Outlook
The U.S. is the only developed country still letting kava be sold freely as a supplement. Canada, the UK, Switzerland, and the entire EU banned it in the early 2000s after liver damage cases piled up. Australia allows it under strict rules. The FDA hasn’t pulled it off the shelves - but they’re watching closely.
In 2024, California issued formal warnings about kava. New York is considering a law that would force warning labels on every product. The NIH just funded $2.4 million to study whether traditional “noble” kava varieties are safer than the commercial types. Early results suggest they might be.
But here’s the real issue: most kava sold online comes from unregulated sources. There’s no standardization. No batch testing. No way to know what’s inside. That’s why 68% of U.S. kava sales happen through Amazon, eBay, or random websites - places where you can’t ask questions.
Meanwhile, kava bars in the U.S. are growing. They serve water-based kava drinks - the kind Pacific Islanders have used for centuries. These are likely safer. But even then, if you’re on medication? Don’t risk it.
Final Advice: When in Doubt, Skip It
Kava isn’t evil. For some people, it helps. But it’s not a harmless herb. It’s a potent substance with real, documented dangers - especially when mixed with medications you’re already taking.
If you’re using kava for anxiety or sleep, talk to your doctor. There are safer, proven options - therapy, SSRIs, melatonin, cognitive behavioral techniques. You don’t need to gamble with your liver.
And if you’re already taking sedatives? Don’t add kava. Not even a little. The risk isn’t worth it. Your liver can’t talk. It won’t warn you until it’s too late.
Can kava cause liver damage even if I don’t take any medications?
Yes. While the risk is lower without other medications, liver damage from kava has been reported in people who took it alone. Cases are rare, but they happen. Most involve long-term use of high doses (over 250 mg daily) or alcohol-extracted products. Water-based traditional preparations carry much lower risk, but no form of kava is completely risk-free.
How do I know if kava is affecting my liver?
Early signs are subtle: unexplained fatigue, nausea, loss of appetite, dark urine, or yellowing of the skin or eyes (jaundice). These symptoms often appear 1 to 4 months after starting kava. By the time they show up, liver damage may already be advanced. The only way to know for sure is a blood test - check ALT, AST, and bilirubin levels. Don’t wait for symptoms.
Is kava safer than prescription anxiety meds?
No. Prescription anxiolytics like alprazolam have a known, very low risk of liver injury - about 1 in 100,000 prescriptions. Kava’s estimated rate is lower, but the problem is unpredictability. Prescription drugs are tested, dosed precisely, and monitored. Kava isn’t. You don’t know what’s in your supplement, how strong it is, or if it’s contaminated. That makes it riskier overall.
Can I take kava if I only use it once a week?
If you’re not on any sedative medications and your liver is healthy, occasional use (once a week) with a low dose (under 100 mg) of water-extracted kava may be low-risk. But “low-risk” isn’t “no-risk.” There’s no proven safe threshold. Experts still recommend avoiding kava entirely if you have any underlying health conditions or are taking other drugs.
What should I tell my doctor if I’ve been taking kava?
Tell them exactly what you’ve been taking: the brand, form (capsule, tea, tincture), daily dose, how long you’ve used it, and whether you’ve combined it with any other drugs or alcohol. Don’t say “I took some herbal stuff.” Be specific. Most doctors won’t ask - so you have to bring it up. It could save your life.