NMS Risk Assessment Tool
Evaluate Your Risk Factors
This tool uses clinical factors from the article to assess potential risk for Neuroleptic Malignant Syndrome. It is not a diagnostic tool and does not replace medical advice.
Important Safety Information
NMS is a medical emergency. If you or someone you know shows symptoms like:
- Stiff muscles (lead pipe rigidity)
- Fever over 100.4°F (38°C)
- Confusion or mutism
- Rapid heart rate or unstable blood pressure
Neuroleptic Malignant Syndrome (NMS) isn’t something most people have heard of - until it happens. And when it does, it’s not a slow, creeping problem. It’s a medical emergency that can turn a stable patient into a critically ill person in under 48 hours. This isn’t just a bad side effect. It’s a life-threatening reaction to certain psychiatric and anti-nausea medications, triggered by a simple but dangerous disruption in brain chemistry. If you or someone you care for is on an antipsychotic, you need to know the signs - because waiting too long can be fatal.
What Exactly Is Neuroleptic Malignant Syndrome?
NMS is a rare but deadly reaction caused by drugs that block dopamine receptors in the brain. These include antipsychotics like haloperidol, risperidone, and olanzapine, but also non-psychiatric drugs like metoclopramide and promethazine, used for nausea and vomiting. The core problem? Dopamine, a chemical that helps control movement, body temperature, and alertness, gets shut down. That’s what triggers the four classic symptoms: muscle rigidity, high fever, confusion or altered mental state, and wild swings in heart rate, blood pressure, and sweating.
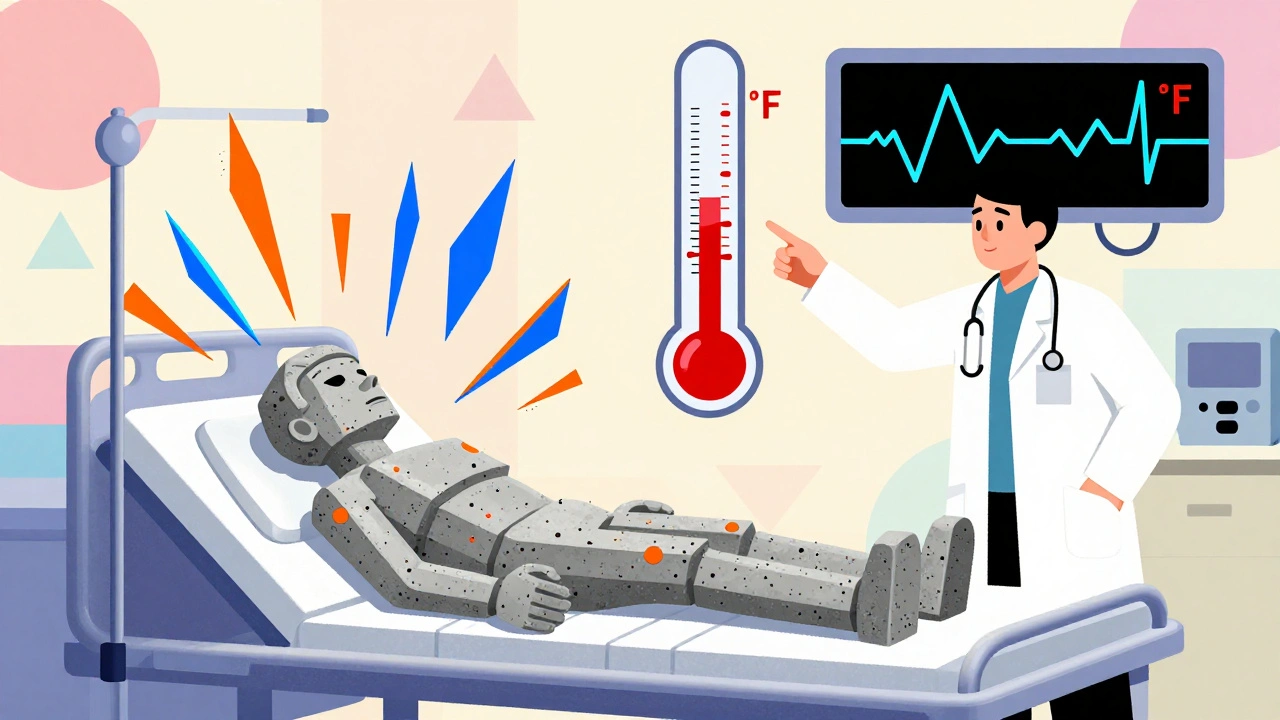
It’s not a guess. Doctors diagnose NMS when all four symptoms are present. Muscle rigidity isn’t just stiffness - it’s lead pipe rigidity, where limbs feel like they’re made of concrete and don’t bend even when someone tries to move them. Fever isn’t a mild 100°F. It’s often above 104°F (40°C). Mental status changes range from agitation to complete mutism - the person can’t speak or respond. Autonomic instability means their body can’t regulate basic functions: heart races, blood pressure spikes or crashes, they sweat profusely or stop sweating altogether.
And here’s the kicker: NMS usually shows up within the first two weeks of starting or increasing a medication. But it can also hit during long-term use - even if the dose hasn’t changed. About 60% of cases occur when someone first starts the drug, 30% when the dose is raised, and 10% when they’ve been on it for months or years.
Why Is NMS So Dangerous?
The danger doesn’t stop at the symptoms. The body starts breaking down muscle tissue - a process called rhabdomyolysis. When muscles break down, they release a protein called myoglobin into the bloodstream. That stuff clogs the kidneys. About 30% of severe NMS cases lead to acute kidney injury. Some patients need dialysis. Others don’t survive.
Lab tests show the damage. Creatine kinase (CK) levels - a marker of muscle breakdown - often shoot above 1,000 IU/L. In extreme cases, they hit 100,000 IU/L. White blood cell counts rise. Blood becomes acidic. Potassium levels climb dangerously high. Iron levels drop. These aren’t just numbers. They’re warning signs that the body is failing.
Without treatment, NMS kills 10 to 20% of patients. Even with treatment, 5% still die. But here’s the good news: if caught early and treated properly, survival rates have jumped to 95%. That’s because we now know exactly what to do - and we know how fast to do it.
How Is NMS Different From Similar Conditions?
Doctors often mistake NMS for other emergencies. That’s dangerous. Two conditions look similar but need totally different treatments: serotonin syndrome and malignant hyperthermia.
Serotonin syndrome happens when too much serotonin builds up - usually from combining antidepressants. It comes on fast - within hours. You see clonus (involuntary muscle spasms), hyperreflexia (overactive reflexes), and diarrhea. NMS? Slower onset - days to weeks. No clonus. Instead, you get lead pipe rigidity and mutism. Fever is higher in NMS. Gastrointestinal symptoms are less common.
Malignant hyperthermia is triggered by anesthesia during surgery. It hits within minutes. You see jaw muscle spasms (masseter spasm), rapid breathing, and dark brown urine from muscle breakdown. NMS doesn’t have the jaw spasm. And it’s not tied to anesthesia - it’s tied to psychiatric or anti-nausea meds.
Confusing these three can cost lives. Giving a serotonin syndrome patient dantrolene (a muscle relaxant used for NMS) won’t help. Giving an NMS patient serotonin-blocking drugs like cyproheptadine might make things worse. Accurate diagnosis isn’t optional - it’s the difference between life and death.
Who’s at Risk?
NMS doesn’t pick favorites, but some people are more vulnerable. Young men are twice as likely to develop it as women. People with bipolar disorder have a higher risk than those with schizophrenia. Rapidly increasing the dose of a high-potency antipsychotic - like jumping haloperidol from 5mg to 15mg in a day - is a major red flag. Giving the drug by injection instead of orally also raises risk.
Using lithium with antipsychotics? That combination triples the risk. Even stopping Parkinson’s meds like levodopa too quickly can trigger NMS. And here’s something many don’t realize: up to 12% of NMS cases happen in people on therapeutic doses with no known risk factors. That means even if you’re doing everything “right,” it can still happen.
Patients with a history of NMS are at high risk of recurrence. If you’ve had it once, you can’t safely take the same class of drugs again. Alternatives must be found.
What Happens When NMS Is Suspected?
There’s no single blood test for NMS. Diagnosis is clinical - based on symptoms, timing, and medication history. But once it’s suspected, time is the enemy. Every hour counts.
Step one: Stop the drug. All of it. No exceptions. Even if the patient is improving, the medication must be discontinued immediately.
Step two: Get to the ICU. NMS needs constant monitoring. Temperature, heart rhythm, kidney function, electrolytes - all tracked hourly. Cooling blankets, IV fluids, and oxygen are started right away.
Step three: Medications. Dantrolene is the go-to muscle relaxant. It’s given intravenously, starting at 1-2.5 mg per kg of body weight, and can be repeated up to 10 mg/kg if needed. Bromocriptine, a dopamine agonist, helps restore brain dopamine levels - usually given orally every 8 hours. In some hospitals, intranasal apomorphine is being tested and has shown promise in lowering fever within 4 hours.
Step four: Protect the kidneys. Hydration is critical. Doctors aim for urine output above 30 mL per hour. If kidneys start failing, dialysis may be needed. Electrolytes are corrected. Acidosis is treated.
Step five: Watch for complications. Infections, blood clots, heart rhythm problems - all common during recovery. Recovery usually takes 7 to 10 days, but muscle weakness can linger for weeks. Some patients take 8 weeks to walk again.

What Happens After Recovery?
Surviving NMS isn’t the end of the story. Many patients are terrified to take any psychiatric medication again. A 2022 survey found 65% of survivors refused to restart antipsychotics, even when their psychosis returned. That creates a cruel dilemma: treat the mental illness, or risk another NMS episode?
Doctors now use a cautious approach. If a patient needs antipsychotics again, they avoid the same drug class entirely. Sometimes, a very low dose of a different antipsychotic - like clozapine - is tried under strict supervision. But many patients never take another neuroleptic. Non-drug therapies like CBT, family support, and mood stabilizers become the focus.
For those who do restart meds, the rule is slow, slow, slow. Dose increases happen over weeks, not days. Monitoring is intense. CK levels are checked every 24 hours for the first week.
What’s Changing in NMS Treatment?
Thanks to second-generation antipsychotics - like quetiapine and aripiprazole - NMS has become far rarer. Where it used to affect up to 2% of people on older drugs like haloperidol, it now affects only 0.01-0.02% on newer ones. That’s a 95% drop.
But the danger hasn’t vanished. In January 2023, the FDA required all antipsychotic labels to include stronger warnings about NMS. The message is clear: even at normal doses, in people with no risk factors, it can still happen.
Research is moving fast. Some hospitals are using AI tools to scan electronic health records for early signs - like a sudden spike in temperature combined with rising CK levels - and alert doctors before symptoms become obvious. One trial found these tools could flag potential NMS cases 24 hours before a human clinician would notice.
Future drugs may target dopamine more precisely, avoiding the full blockage that causes NMS. If successful, this could make the syndrome nearly extinct within the next decade.
What Should You Do If You Suspect NMS?
If you’re on an antipsychotic or anti-nausea drug and suddenly develop:
- Stiff muscles that feel like concrete
- Fever over 100.4°F (38°C)
- Confusion, mutism, or agitation
- Rapid heartbeat, sweating, or unstable blood pressure
Call 911 or go to the ER immediately. Tell the staff: “I’m on an antipsychotic or dopamine-blocking drug. I think I might have Neuroleptic Malignant Syndrome.” Don’t wait. Don’t assume it’s just a bad reaction or worsening psychosis. NMS is not a psychiatric issue - it’s a medical emergency.
And if you’re a caregiver, don’t hesitate to speak up. Many cases are missed because staff assume the patient is just “acting out.” Muscle rigidity and fever are not normal. They’re red flags.
Can NMS happen with non-psychiatric drugs?
Yes. While antipsychotics are the most common cause, NMS can also be triggered by anti-nausea drugs like metoclopramide and promethazine. These are dopamine blockers too. About 15% of NMS cases are linked to these medications, not psychiatric drugs. Even over-the-counter motion sickness patches containing scopolamine have been linked to rare cases.
How long does it take to recover from NMS?
Most patients recover physically within 7 to 10 days if treated early. But full recovery can take weeks. Muscle weakness, fatigue, and cognitive fog often linger. Some patients report taking up to 8 weeks to walk normally again. Long-term muscle damage is rare but possible - especially if treatment was delayed.
Is NMS more common in certain age groups?
It’s most common in young and middle-aged adults, with a higher rate in males - about 2:1 compared to females. It’s rare in children and older adults, but not impossible. The biggest risk factor isn’t age - it’s rapid dose increases and the type of medication used.
Can you get NMS from stopping a medication?
Yes. Rapidly stopping Parkinson’s medications like levodopa can trigger NMS. This accounts for about 5% of cases. The body suddenly loses dopamine stimulation, which mimics the effect of blocking dopamine receptors. Symptoms appear within 24 to 72 hours after stopping the drug.
Are there any long-term effects after surviving NMS?
Most people recover fully, but about 15% have lingering muscle weakness or movement issues at 30 days. Some report chronic fatigue or difficulty concentrating. Psychological trauma from the ICU experience is common. A small number develop permanent kidney damage if they had severe rhabdomyolysis. Regular follow-up with a neurologist is recommended.
Can NMS be prevented?
Yes, to a large extent. Avoid rapid dose increases. Don’t combine dopamine blockers unless absolutely necessary. Use second-generation antipsychotics when possible - they’re much safer. Monitor CK levels during the first two weeks of starting a new antipsychotic. Educate patients and caregivers about the warning signs. Early recognition saves lives.
If you’re managing someone on antipsychotics, keep a list of symptoms to watch for. Write them down. Share them with the care team. NMS is rare - but when it strikes, it doesn’t give second chances. Knowledge is your best defense.


December 11, 2025 AT 13:22 PM
I work in ER and seen this twice. One guy on metoclopramide for nausea just went from fine to rigid and feverish in 18 hours. We almost missed it because no one thought a simple anti-nausea drug could do this. Thank you for writing this. Everyone needs to know.
December 12, 2025 AT 04:57 AM
This is why I refuse to take anything psychotropic. My cousin died from this after being prescribed risperidone for "anxiety." They called it a "bad reaction." It was murder by protocol.
December 13, 2025 AT 12:01 PM
I'm a nurse who's seen NMS up close. The scariest part? The silence. Patients don't scream. They just... stop. No movement. No response. Just heat and rigidity. And if you don't catch it before CK hits 5000, you're racing the clock. I wish every prescriber had to sit through a 72-hour NMS crash like I have.
December 13, 2025 AT 23:32 PM
So let me get this straight. You're telling me that a drug meant to calm the mind can literally turn your body into a furnace and your muscles into concrete? And we're still prescribing these like candy? What even is modern medicine anymore?
December 14, 2025 AT 23:32 PM
I bet this is just big pharma scare tactics. People get sick all the time. This is just another way to make doctors paranoid and sell more tests. My uncle took haloperidol for 10 years and never had an issue.
December 16, 2025 AT 02:34 AM
The part about dopamine blockade being the core mechanism is spot on. It's not just about psychosis-it's about motor control, thermoregulation, autonomic function. All dopamine-dependent. That's why the symptoms cluster the way they do. This is textbook neuropharmacology in action.
December 17, 2025 AT 23:57 PM
dude i read this whole thing and still dont get why we dont just stop giving these drugs period. like if it can kill you in 2 days and you dont even know its coming... why risk it? just give them yoga and vibes bro
December 18, 2025 AT 14:53 PM
My sister had this after a single IV dose of promethazine. She was in ICU for 11 days. We didn’t know what was happening until the nurse said, "This looks like NMS." No one else did. Please, if you’re on any of these meds, print this out and give it to your doctor. Knowledge is power.
December 19, 2025 AT 15:50 PM
In India we see this less often but still exist. Many doctors still use haloperidol injections like it's nothing. I showed this to my cousin who works in a rural hospital. He said he'll start training his staff. Small change matters.
December 20, 2025 AT 19:52 PM
I used to work in psych wards. The worst part wasn't the fever or the rigidity-it was the guilt. We'd see patients deteriorate and think "it's just psychosis getting worse." We didn't know. Now I carry a printed checklist in my pocket. No one should die because we assumed.
December 22, 2025 AT 14:21 PM
So you're saying a 10mg dose of olanzapine can kill someone? That's ridiculous. If your body can't handle a little antipsychotic, maybe you shouldn't be on it.
December 23, 2025 AT 00:50 AM
I think the real tragedy isn't just the syndrome-it's how invisible it is to the people who aren't trained to see it. Families think their loved one is "acting out." Nurses think it's delirium. Doctors think it's infection. It's a perfect storm of normalcy masking catastrophe.
December 24, 2025 AT 08:09 AM
The AI monitoring systems mentioned are already live in some major hospitals. One system flagged a patient in real-time because CK spiked 400% in 8 hours while temp hit 103.5°F. The team responded before the patient even became rigid. Tech saving lives? Unbelievable.
December 25, 2025 AT 02:14 AM
I'm a caregiver for my dad with bipolar. He's on quetiapine now. I keep a thermometer, a notebook, and this article in his wallet. If he gets stiff or hot, I call 911 before I call the doctor. Better safe than sorry.
December 25, 2025 AT 14:15 PM
We treat dopamine like it's a switch you flip on and off. But the brain isn't a lightbulb. It's a symphony. Block one note, and the whole piece collapses. NMS isn't a side effect-it's the sound of a system screaming when you pull its foundation out.
December 27, 2025 AT 07:08 AM
This is an excellent summary. I will be sharing this with our internal medical education team. The distinction between serotonin syndrome and NMS is critical and often misapplied in triage.
December 28, 2025 AT 12:53 PM
Yeah but what about the people who actually need these meds? You're just gonna leave them untreated? That's worse.
December 28, 2025 AT 20:36 PM
I'm so glad someone finally wrote this without fear. I used to work in pharmacy and saw too many scripts get filled without a second thought. This isn't just info-it's a lifeline.
December 29, 2025 AT 13:53 PM
I'm not a doctor but I've had 3 family members on antipsychotics. I'm printing this and taping it to the fridge. 🚨
December 31, 2025 AT 09:48 AM
If you're on any dopamine-blocking drug and your muscles feel like they're turning to stone, don't wait for a doctor. Go to the ER. Now.