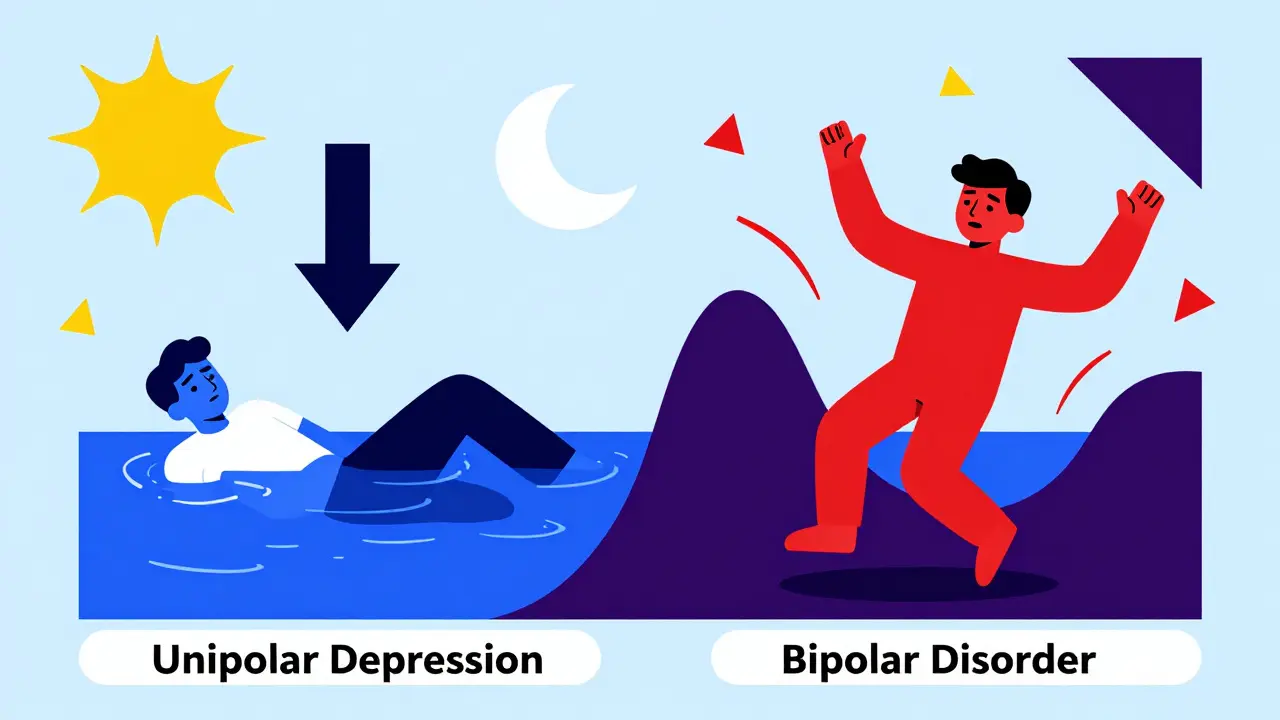
When someone feels persistently low, tired, and hopeless, it’s easy to assume they have depression. But not all depression is the same. Bipolar depression and unipolar depression look alike on the surface - both involve deep sadness, loss of energy, and trouble sleeping. Yet they’re fundamentally different conditions, and mistaking one for the other can lead to dangerous treatment mistakes.
What Exactly Is the Difference?
Unipolar depression, also called Major Depressive Disorder (MDD), means a person experiences only depressive episodes. No highs. No energy surges. No periods of reckless behavior or extreme confidence. It’s a one-way mood slide - down. Bipolar depression is different. It’s not a standalone illness. It’s the low phase of bipolar disorder. People with bipolar disorder swing between depression and mania (or hypomania). Mania means elevated mood, racing thoughts, little need for sleep, impulsive spending, or risky behavior. Hypomania is a milder version, but still noticeable and disruptive. If someone has ever had even one manic or hypomanic episode, they have bipolar disorder - even if they spend most of their time depressed. This distinction isn’t just academic. It changes everything about treatment. Giving an antidepressant to someone with bipolar depression can trigger mania, rapid cycling, or worsen their illness long-term.How Doctors Tell Them Apart
Diagnosing correctly starts with asking the right questions. Many people with bipolar disorder are misdiagnosed as having unipolar depression - sometimes for years. A 2018 study found that 37% of people with bipolar disorder were initially labeled as having unipolar depression. Doctors look for clues:- Family history: If a close relative has bipolar disorder, the risk jumps from 1-2% in the general population to 5-10%.
- Early age of onset: First depressive episodes before age 25 are more common in bipolar disorder.
- Atypical symptoms: Sleeping too much (hypersomnia), feeling heavy or numb (leaden paralysis), and intense sensitivity to rejection are more frequent in bipolar depression.
- Antidepressant response: If someone had a bad reaction to an antidepressant - like sudden agitation, impulsivity, or mania - it’s a red flag for bipolar disorder.
- Episode patterns: Rapid cycling (four or more mood episodes in a year) almost always points to bipolar disorder.
Treatment: Why One Size Doesn’t Fit All
This is where things get critical. Treatment for unipolar depression is straightforward: antidepressants are the first line. SSRIs like sertraline or escitalopram help about 60-65% of people within 8-12 weeks. But for bipolar depression? Antidepressants alone are risky. The STEP-BD study showed that 76% of people with bipolar disorder who took antidepressants without a mood stabilizer had their mood destabilized - some into full-blown mania. Instead, bipolar depression treatment focuses on mood stabilizers and atypical antipsychotics:- Lithium: One of the oldest and most studied treatments. It reduces depressive symptoms in about 48% of cases, compared to 28% with placebo.
- Quetiapine (Seroquel): Approved specifically for bipolar depression. In trials, 58% responded, versus 36% on placebo.
- Lurasidone (Latuda): Also FDA-approved for bipolar depression, with strong evidence for reducing symptoms without triggering mania.
What Happens When You Get It Wrong?
Misdiagnosis isn’t just inconvenient - it’s harmful. A 2017 study found that people misdiagnosed with unipolar depression when they actually had bipolar disorder spent an average of 8.2 years on the wrong treatment. During that time, 63% had at least one hospitalization because antidepressants triggered mania. Real stories back this up. On Reddit’s r/bipolar, 78% of 1,243 respondents said they were first told they had unipolar depression. One user wrote: “I was on Prozac for seven years. My mood cycles went from two episodes a year to twelve. My psychiatrist finally noticed - I was hypomanic every time I got a prescription refill.” The financial cost is heavy too. A 2021 study estimated that misdiagnosed bipolar patients cost the healthcare system $13,247 more per year due to hospital stays and medication changes.Long-Term Management
Unipolar depression often allows for stopping medication after 6-12 months of remission - especially if it’s the first episode. Many people never have another episode. Bipolar disorder is different. It’s a lifelong condition. Stopping mood stabilizers? The relapse rate jumps to 73% within five years. With continued treatment, it drops to 37%. That’s why lithium, lamotrigine, or quetiapine are often taken indefinitely - not because the person is “broken,” but because the illness requires ongoing management.
New Hope on the Horizon
Research is moving fast. In 2019, the FDA approved esketamine (Spravato) for treatment-resistant unipolar depression. It works fast - some feel better in hours. For bipolar depression, cariprazine (Vraylar) was approved the same year, with 37% of patients achieving remission in 8 weeks. Even more promising: a 2023 study in Lancet Psychiatry identified a 12-gene pattern that distinguishes bipolar from unipolar depression with 83% accuracy. Blood tests may one day help confirm diagnosis. Digital tools are also emerging. Apps that track sleep, speech patterns, and typing speed through smartphones can detect subtle mood shifts before they become full episodes.What Should You Do?
If you’ve been diagnosed with depression and:- Have a family history of bipolar disorder
- Had a bad reaction to an antidepressant
- Experienced periods of unusually high energy or impulsivity
- Have frequent mood swings
- Are still struggling after trying two or more antidepressants
Can you have bipolar disorder without ever being manic?
No. By definition, bipolar disorder requires at least one manic or hypomanic episode. If someone has only depressive episodes, they’re diagnosed with unipolar depression. However, many people don’t recognize their hypomanic episodes as abnormal. They might feel “more productive” or “more social” during those times and never mention them to a doctor. That’s why it’s critical to ask about past periods of unusually high energy, reduced sleep, or impulsive behavior.
Are antidepressants always dangerous for bipolar depression?
Not always - but they’re risky as a standalone treatment. Antidepressants can trigger mania, rapid cycling, or worsen mood instability. The American Psychiatric Association and NICE guidelines strongly advise against using them alone. However, if mood is stabilized first with lithium, quetiapine, or another mood stabilizer, antidepressants may be cautiously added for persistent depressive symptoms. Even then, they’re used sparingly and monitored closely.
How long does it take to get the right diagnosis?
On average, it takes 7 to 10 years from first symptoms to correct bipolar diagnosis. Many people see multiple doctors, try several medications, and experience multiple hospitalizations before someone connects the dots. The delay is often because depression is the most visible symptom, and manic episodes may be rare, mild, or forgotten. Screening tools like the MDQ and HCL-32 can help speed this up.
Is bipolar depression more severe than unipolar depression?
It’s not necessarily more severe - but it’s more complex. People with bipolar depression often have more intense symptoms: higher rates of psychosis, early morning waking, psychomotor slowing, and suicidal thoughts. They also cycle between extremes, which makes daily life harder to manage. The risk of suicide is higher in bipolar disorder than in unipolar depression, especially during depressive phases. But both conditions are serious and require professional care.
Can lifestyle changes help with bipolar depression?
Yes - but they’re not a replacement for medication. Regular sleep, consistent meals, avoiding alcohol, and managing stress are essential. In fact, Interpersonal and Social Rhythm Therapy (IPSRT) is built around this. Keeping a steady daily routine helps prevent mood episodes. Exercise, sunlight, and mindfulness can support treatment, but they won’t stop mania or deep depression on their own. Medication and therapy are still the foundation.


February 20, 2026 AT 21:03 PM
Depression isn’t a diagnosis. It’s a symptom. And we’re still treating it like a light switch instead of a dimmer.
Stop prescribing SSRIs like they’re aspirin.