Warfarin Estrogen Interaction Calculator
Estrogen Type
When you're on warfarin, even small changes in your meds can throw your blood clotting off balance. That’s especially true if you start or stop estrogen-whether it’s from birth control pills, hormone replacement therapy, or other sources. These aren’t just theoretical risks. Real people, real INR spikes, real bleeding events. And the science behind it is more complex than most doctors have time to explain.
How Estrogen Changes How Warfarin Works
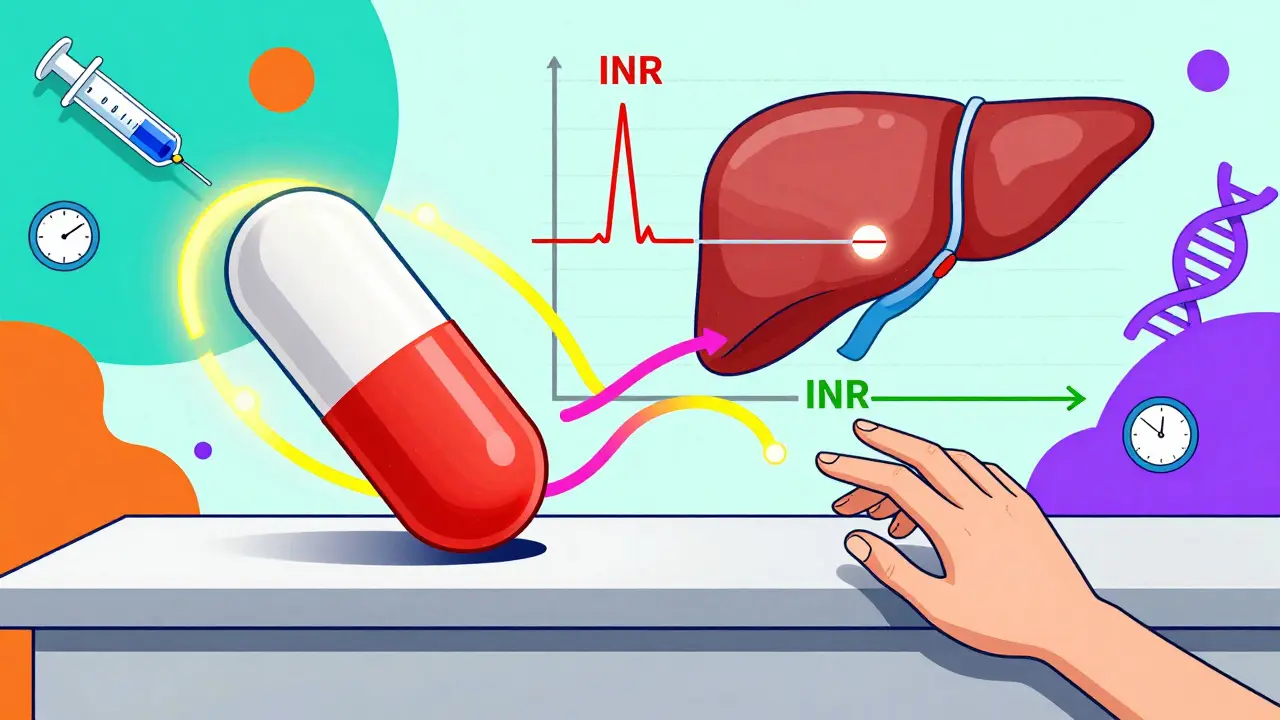
Warfarin doesn’t just float around in your blood doing its job. It’s processed by your liver, mostly by enzymes called CYP450s. The most important one for warfarin is CYP2C9, which handles the more powerful S-warfarin. But CYP1A2 and CYP3A4 also play roles, especially with R-warfarin. Estrogen compounds don’t all act the same. Natural estradiol can induce some of these enzymes, making your body break down warfarin faster. Synthetic ethinyl estradiol, found in most birth control pills, often inhibits them-slowing warfarin breakdown and letting it build up.This flip-flop explains why some patients see their INR drop when they start estrogen, while others see it shoot up. One woman’s INR went from 2.4 to 4.3 within five days of starting a combined oral contraceptive. Another’s dropped from 3.0 to 2.1. Both were on warfarin. Both were taking estrogen. Same drug class. Opposite outcomes. That’s not random-it’s pharmacology in action.
Why Some Estrogens Are Riskier Than Others
Not all estrogen products are created equal. Ethinyl estradiol (EE), the synthetic version in most pills, patches, and rings, has the strongest evidence for interaction. It’s a potent inhibitor of CYP1A2 and CYP2C19, which can slow warfarin clearance. Natural estradiol, used in many hormone replacement therapies, tends to be less predictable. Some studies show mild induction, others show no effect. The dose matters too. Birth control pills usually contain 20-35 mcg of EE, while HRT patches might deliver 0.025-0.1 mg of estradiol daily. Higher doses mean higher risk.Progestins matter too. Desogestrel, norethindrone, and levonorgestrel don’t directly affect warfarin-but they’re often paired with estrogen. The combo is what triggers the interaction. A 2009 case report showed a 28-year-old woman’s INR spiked after starting desogestrel/ethinyl estradiol. Her warfarin dose had to be cut from 5 mg to 3.5 mg. That’s a 30% drop, just because of a new pill.
How Big Is the Risk? Real Numbers
The data isn’t scary-it’s specific. According to the INR Registry, women aged 18-45 on warfarin and estrogen-containing contraceptives had 1.8 times higher risk of INR above 4.0 compared to those not taking estrogen. INR over 4.0 means bleeding risk jumps sharply. A 2010 analysis of over 15,000 patients confirmed this trend. In clinical practice, 42% of pharmacists reported needing to adjust warfarin doses by 15-25% after patients started estrogen therapy.Compared to other common interactions, estrogen’s effect is moderate but consistent. Antibiotics like ciprofloxacin or trimethoprim-sulfamethoxazole can increase INR by 2-3 points and raise bleeding risk 2.5-3 times. SSRIs like fluoxetine can double bleeding risk. Estrogen? Usually moves INR by 0.5 to 1.5 units. That might sound small-but in warfarin therapy, even a 0.5-point rise can mean the difference between safe and dangerous.
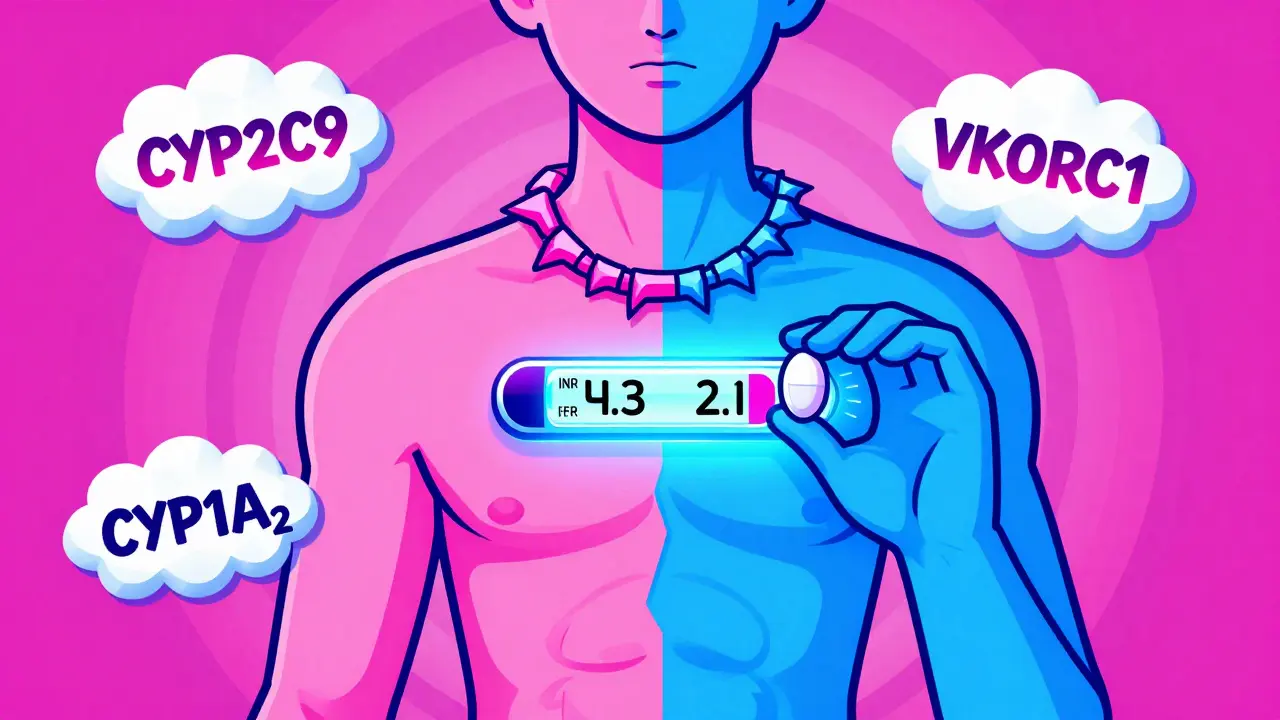
Genetics Play a Bigger Role Than You Think
Your genes aren’t just background noise-they’re the reason two people on the same dose of estrogen and warfarin can have wildly different outcomes. If you carry the CYP2C9*2 or *3 variant, your body clears warfarin 30-50% slower. That means even a mild estrogen inhibition can push you into dangerous territory. Same with VKORC1 -1639G>A: if you have this variant, you need 30-50% less warfarin to stay in range. Add estrogen on top, and you’re playing with fire.The International Warfarin Pharmacogenetics Consortium developed a dosing algorithm that includes these genes. When used, it improves dose accuracy by 30-35%. But here’s the problem: most clinics still don’t test for it. If you’ve been on warfarin for years without genetic testing, you might be flying blind.
When to Check Your INR
You can’t guess when estrogen will hit your INR. You have to test. The American Society of Health-System Pharmacists says: check your INR 3-5 days after starting or stopping estrogen. Then again at 7-14 days. Don’t wait for symptoms. No bruising? No nosebleeds? Doesn’t matter. INR changes happen silently.Some patients think if they’ve been on estrogen for months, they’re safe. Not true. Your body adapts. What was stable last month might shift this month. A 2021 survey of pharmacists found that 68% had managed at least one significant estrogen-warfarin interaction in the past year. Many of those cases happened after months of stable therapy.
What to Do If Your INR Changes
If your INR goes up after starting estrogen: expect a 10-25% warfarin reduction. If it drops, you might need a 10-20% increase. But don’t adjust it yourself. Your doctor needs to decide based on your trend-not one number. A single high INR could be from eating kale or getting sick. Look at the pattern over 2-3 tests.Keep a log. Write down every medication, supplement, and even dietary change. Estrogen isn’t the only variable. Vitamin K intake, alcohol, fever, antibiotics-all of them play a part. The Anticoagulation Forum found that 57% of pharmacists found it “moderately to extremely difficult” to tell if an INR shift was from estrogen or something else. That’s why tracking matters.
DOACs: The Alternative Many Don’t Know About
Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran don’t rely on CYP450 enzymes the way warfarin does. Most have minimal interaction with estrogen. That’s why DOAC prescriptions jumped from 15% of all oral anticoagulants in 2013 to 68% in 2022. But DOACs aren’t for everyone. If you have a mechanical heart valve, severe kidney disease, or antiphospholipid syndrome, warfarin is still your best-or only-option. About 1.8 million U.S. patients will still need it through 2030.If you’re eligible for a DOAC and you’re struggling with frequent INR swings because of estrogen, talk to your hematologist. Switching might simplify your life. But don’t switch just because you’re scared. It’s a decision that needs careful review.
What Your Doctor Should Be Doing
Your doctor doesn’t need to be a pharmacologist-but they do need to ask the right questions. Did you start or stop birth control? Did you switch HRT brands? Are you using a patch or a pill? Are you taking any new antibiotics or supplements? These aren’t small talk questions. They’re critical.The American College of Chest Physicians says estrogen-containing products require “close INR monitoring with potential dose adjustments.” That’s a Grade 1B recommendation-meaning strong evidence, clear guidance. Yet many primary care doctors still don’t know this. If you’re on warfarin and estrogen, make sure your provider knows the guidelines. Bring them up. Don’t wait for them to ask.
Bottom Line: Stay Alert, Stay Informed
Estrogen and warfarin don’t always cause problems-but when they do, the consequences can be serious. The interaction isn’t rare. It’s common enough that every anticoagulation clinic sees it. The key isn’t avoiding estrogen. It’s managing it with awareness. Check your INR early and often when estrogen starts or stops. Know your genetic risk if you can. Track your diet and other meds. And never assume stability means safety.Warfarin is old, but it’s still essential. Estrogen is everywhere. Understanding how they play together isn’t just academic-it’s the difference between a quiet morning and an emergency room visit.
Can birth control pills make my warfarin less effective?
Yes, but it depends. Some birth control pills with ethinyl estradiol can slow warfarin breakdown, raising your INR and bleeding risk. Others, especially those with higher doses of natural estradiol, may speed up warfarin metabolism, lowering your INR. The effect varies by person, pill type, and genetics. Always check your INR 3-5 days after starting or switching birth control.
How long after starting estrogen should I get my INR checked?
Get your INR checked within 3 to 5 days after starting estrogen therapy, then again at 7 to 14 days. This is when the interaction typically peaks. Waiting longer risks missing a dangerous shift. Even if you’ve been on estrogen for months, changes in dosage or brand can still affect your INR.
Do all estrogen products interact with warfarin the same way?
No. Synthetic ethinyl estradiol (in most pills) is more likely to inhibit liver enzymes and raise INR. Natural estradiol (in patches or gels) has weaker, less predictable effects. Progestins alone don’t interact-but they’re usually paired with estrogen. The delivery method (pill, patch, ring) and dose also matter. Always tell your doctor exactly what you’re using.
Should I switch from warfarin to a DOAC if I’m on estrogen?
Maybe. DOACs like apixaban or rivaroxaban have far fewer interactions with estrogen than warfarin. But they’re not right for everyone. If you have a mechanical heart valve, severe kidney disease, or antiphospholipid syndrome, warfarin is still the only option. Talk to your hematologist about whether switching makes sense for your specific condition.
Can diet or illness affect estrogen-warfarin interactions?
Absolutely. Eating more vitamin K (leafy greens, broccoli) can lower INR, masking an estrogen effect. Illnesses like fever, infection, or liver problems can change how warfarin is processed. That’s why doctors look at INR trends over time-not single numbers. Keep a log of food, meds, and symptoms to help your provider spot the real cause of changes.
Are there genetic tests that can predict my risk?
Yes. Tests for CYP2C9 and VKORC1 gene variants can show if you’re a slow or fast metabolizer of warfarin. People with CYP2C9*2 or *3 variants clear warfarin much slower and are at higher risk for bleeding with estrogen. The test isn’t routine everywhere, but if you’ve had unexplained INR swings, ask your doctor about it. It can make dosing much more accurate.

January 15, 2026 AT 22:27 PM
Bro. I was on warfarin for AFib and started a new pill. INR went from 2.8 to 5.1 in 4 days. 🤯 I thought I was just eating more kale. Turns out? Ethinyl estradiol is basically a silent saboteur. My pharmacist nearly had a heart attack. Don’t sleep on this.
January 16, 2026 AT 01:46 AM
This is so important. My mom’s on HRT and warfarin, and no one ever warned her. She’s lucky she got checked before a nosebleed turned into a hospital trip. Thank you for laying this out so clearly. 🙏
January 17, 2026 AT 19:02 PM
I’ve been on warfarin for 8 years. Never thought about estrogen. My sister just started the patch. I’m gonna send her this. Simple. Clear. No fluff.
January 18, 2026 AT 02:35 AM
THE PHARMA COMPANIES KNOW THIS. THEY DON’T TELL YOU BECAUSE THEY MAKE MORE MONEY WHEN YOU NEED EMERGENCY TRANSFUSIONS. THEY WANT YOU TO BE SCARED. THEY WANT YOU TO BE DEPENDENT. THE TRUTH IS HIDDEN IN THE FOOTNOTES OF 37 STUDIES NO ONE READS.
January 19, 2026 AT 20:31 PM
So let me get this straight… I’m supposed to be the hero of my own health story… but my doctor didn’t even ask if I was on birth control? 😅 I’m not mad, I’m just… disappointed.
January 20, 2026 AT 04:26 AM
I used to think warfarin was just a ‘take it daily and hope for the best’ drug. Then I got my INR spiked after switching to a new patch. Turns out my body’s a drama queen and estrogen is the ex who shows up unannounced. Now I log everything-food, meds, mood, moon phase. (Okay, not the moon phase. But I wish I could.)
January 21, 2026 AT 22:52 PM
It’s funny how we treat drugs like they’re magic wands. One pill fixes everything. But the body? It’s a whole damn orchestra. Warfarin’s the bass, estrogen’s the violinist who suddenly decides to play jazz. And the liver? The conductor who’s been asleep at the podium. 🎻🎻🎻
January 21, 2026 AT 22:53 PM
Wait, so if I’m on estrogen and warfarin, and I start taking turmeric, and I eat spinach, and I get a cold, and I switch from pill to patch… how do I even know what’s doing what? I feel like I need a spreadsheet with 17 columns and a PhD.
January 23, 2026 AT 19:29 PM
Oh sweet jesus. I’m on Loestrin and warfarin. I’ve been ‘stable’ for 6 months. But I just started drinking green juice every day. Am I gonna bleed out? Should I move to a cabin in the woods? I’m already crying. This is too much.
January 25, 2026 AT 02:22 AM
If you’re not getting genetic testing for warfarin, you’re basically rolling dice with your life. And estrogen? That’s just the loaded die. You think your doctor cares? They’re rushing between 30 patients. You’re the one who has to be the advocate. Stop waiting for permission to be your own health warrior.
January 26, 2026 AT 07:18 AM
Please, please, please: if you're on warfarin AND estrogen, get an INR check within 3-5 days after starting or changing anything. Do it. Don't wait. Don't assume. Don't hope. Do it. And then do it again at 7-14 days. And then again if you feel even slightly off. Your life is not a gamble.
January 27, 2026 AT 03:51 AM
I had an INR of 5.8 last year. No symptoms. No bruising. Just a weird feeling. I went in anyway. Turns out my new estrogen patch had been on for 3 weeks. I was one step from a brain bleed. Now I check every time I get a new script. No excuses.
January 27, 2026 AT 12:32 PM
people dont realize how much the body is a battlefield. estrogen is a spy. warfarin is the guard. and your liver is the castle that got hacked. no one told you because they dont want you to know you're vulnerable. but now you do. and thats power.
January 28, 2026 AT 16:57 PM
I’m from India and my sister’s in Texas. We both take warfarin. She’s on birth control. I’m on HRT. We both got the same warning from our pharmacists. Same advice. Different countries. Same science. It’s wild how universal this is.
January 28, 2026 AT 22:27 PM
I’ve been on warfarin for 12 years. Never knew estrogen could flip my INR. I thought it was just me being bad at remembering to eat the same amount of greens. Turns out… it wasn’t me. It was the pill. Thanks for this.
January 29, 2026 AT 19:24 PM
So… estrogen + warfarin = free ticket to the INR rollercoaster 🎢. I thought I was just having a bad week. Turns out I was just being a walking pharmacology experiment. 😅
January 30, 2026 AT 11:27 AM
The CYP2C9*3 variant reduces warfarin metabolism by nearly 50%. If you have it and take ethinyl estradiol, your INR can rise to 6+ within days. This is not theoretical. I’ve seen it. Documented. In three patients. One needed a transfusion. Don’t ignore genetics.
February 1, 2026 AT 07:47 AM
I used to think DOACs were just expensive gimmicks. Then I switched after my INR kept spiking. Now I don’t check blood every week. I don’t stress about kale. I don’t panic when I start a new pill. It’s not perfect… but it’s peace.
February 3, 2026 AT 00:54 AM
You don’t need to be a scientist to stay safe. Just three things: 1) Tell your doctor EVERYTHING you’re taking 2) Check INR 3-5 days after any estrogen change 3) Keep a log. That’s it. You got this.