Heart Medication Interaction Checker
This tool helps identify dangerous combinations between common heart medications and other drugs. It's based on the 7 most dangerous combinations documented in medical research. Note: This is not medical advice. Always consult your healthcare provider.
Check for Dangerous Combinations
Important Safety Tips
- 1 Always keep a current list of all medications and supplements
- 2 Use one pharmacy for all prescriptions
- 3 Ask your pharmacist about potential interactions
- 4 Review Beers Criteria for high-risk combinations
- 5 Bring your medication list to every doctor appointment
More than 1 in 3 adults over 65 in the U.S. take five or more prescription drugs every week. For many, that includes heart medications - drugs meant to keep them alive. But what happens when those drugs interact? The results aren’t just inconvenient. They can be deadly.
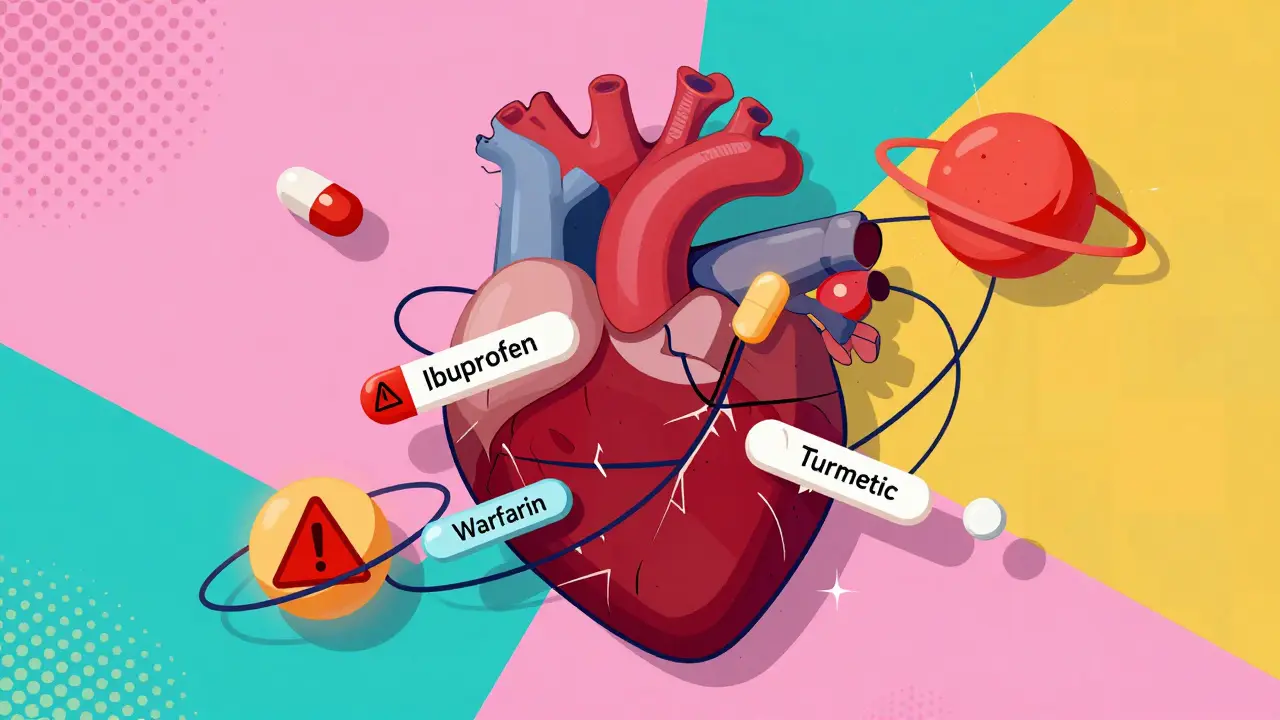
Why Heart Medication Combinations Are So Risky
Heart medications don’t work in isolation. They affect your blood pressure, heart rhythm, kidney function, and blood clotting - all systems that talk to each other. When you add another drug on top, even something as simple as ibuprofen or a vitamin supplement, you can accidentally overload one of those systems.A 2023 study from the USC Schaeffer Center found that taking just two medications with known cardiovascular side effects doubled the risk of heart attack, stroke, or death - even in people with no prior heart disease. Triple the medications? Risk jumped by 218%. And these aren’t rare cases. Adverse drug reactions are the fourth leading cause of death in the U.S., with over 100,000 deaths each year linked to medication interactions.
The 7 Most Dangerous Combinations
Not all drug combos are equal. Some are quietly deadly. Here are the seven most dangerous pairings you need to know:- Warfarin and ibuprofen: Warfarin thins your blood. Ibuprofen irritates your stomach lining. Together, they increase your risk of a serious gastrointestinal bleed by 300%. Many people take ibuprofen for arthritis or back pain without realizing it’s mixing with their blood thinner. One patient in Perth reported bleeding after a routine dental cleaning - she’d been taking Advil daily for years.
- Warfarin and acetaminophen (Tylenol): Unlike ibuprofen, acetaminophen doesn’t hurt your stomach. But long-term use with warfarin can push your INR (a blood clotting measure) up by 2-3 points. That’s enough to cause internal bleeding without warning.
- PDE-5 inhibitors (like Viagra) and nitrates: These are often prescribed for erectile dysfunction and chest pain, respectively. Together, they can crash your blood pressure to dangerously low levels - below 70 mmHg systolic. This isn’t theoretical. Emergency rooms see multiple cases each year from patients who didn’t tell their cardiologist they were taking Viagra.
- Statins and amiodarone: Statins lower cholesterol. Amiodarone controls irregular heartbeat. But when taken together, they increase the risk of muscle damage (myopathy) by 400-500%. This can lead to kidney failure from muscle breakdown products flooding your system.
- ACE inhibitors and potassium supplements: ACE inhibitors help your heart by relaxing blood vessels. But they also cause your body to hold onto potassium. Add a potassium pill or salt substitute, and your levels can spike past 5.5 mEq/L. At that point, your heart can suddenly stop beating. A 2021 study found 18.7% of patients on this combo developed dangerous hyperkalemia - nearly five times higher than those not taking both.
- Digoxin and verapamil: Digoxin slows your heart rate. Verapamil, a calcium channel blocker, does the same. When combined, digoxin levels in your blood rise by 60-75%. That’s enough to cause nausea, confusion, vision changes, and fatal arrhythmias. This combo is especially risky in older adults with reduced kidney function.
- NSAIDs and blood pressure meds: Diclofenac, naproxen, ketorolac - these NSAIDs don’t just cause stomach issues. They make your body hold onto water and salt, raise your blood pressure, and reduce the effectiveness of diuretics and ACE inhibitors by 25-30%. A 2022 survey found 28% of heart patients had taken NSAIDs with their blood pressure meds - often without their doctor knowing.
What About Supplements? They’re Not Always Safe
Many people think “natural” means “safe.” That’s not true - especially with heart meds.St. John’s wort, a common supplement for depression, can slash warfarin levels by up to 50%. That means your blood won’t thin enough - and you could get a clot. Turmeric, ginger, and garlic supplements also thin the blood. One patient in a Reddit heart failure group said his INR shot to over 8.0 after taking turmeric capsules for joint pain. He ended up in the ER with internal bleeding.
Even fish oil, often recommended for heart health, can increase bleeding risk when taken with warfarin or aspirin. And magnesium supplements? They can interfere with digoxin absorption.
There’s no such thing as a “harmless” supplement when you’re on heart medication. Always check with your pharmacist before adding anything new - even if it’s sold in a health food store.

What’s Safe? The Good Combinations
Not all combos are bad. Some are life-saving.Statins, aspirin, and beta blockers together reduce death risk by 25-30% in high-risk patients - a proven combo for decades. Newer drugs like SGLT2 inhibitors (dapagliflozin, empagliflozin) are now being added to standard heart failure regimens and have been shown to cut cardiovascular events by 14%.
And here’s something promising: fixed-dose “polypills” - single pills that combine three proven medications (like a statin, blood pressure drug, and aspirin) - are now being tested in real-world settings. A 2023 study showed patients on polypills were 22% more likely to stick with their treatment and had 15% fewer hospital visits.
How to Protect Yourself
You don’t need to be a medical expert to avoid dangerous combinations. Just follow these steps:- Keep a current list. Write down every pill, patch, cream, and supplement you take - including doses and how often. Don’t say “blood pressure pill.” Say “lisinopril 10 mg once daily.” Update it every 30 days.
- Use one pharmacy. All your prescriptions - even over-the-counter stuff - should come from the same pharmacy. Their system flags dangerous combos automatically.
- Ask your pharmacist. Pharmacists are trained to catch interactions. When you pick up a new prescription, ask: “Could this interact with anything else I’m taking?”
- Know your Beers Criteria. The American Geriatrics Society updated its list in 2023 - it identifies 30 high-risk combinations for people over 65. Ask your doctor if any of your meds are on it.
- Bring your list to every appointment. Don’t assume your doctor remembers what you took last month. Bring the updated list. Even if you’ve seen the same doctor for years.

Why Doctors Miss These Interactions
It’s not that doctors are careless. They’re overwhelmed.A 2023 report found only 37% of primary care doctors routinely screen for dangerous drug combos during visits. Why? Time. Most appointments are 10-15 minutes. And many patients don’t mention supplements or OTC meds unless asked directly.
Plus, electronic health records aren’t perfect. They catch about 85-92% of known interactions - but miss the ones involving supplements, herbal products, or recent changes patients didn’t report.
Medicare Part D now covers 30-minute Medication Therapy Management (MTM) sessions for free. If you’re on multiple heart meds, ask your pharmacist about scheduling one. It’s a simple way to catch problems before they cause harm.
The Future: Better Tools, Fewer Mistakes
The system is slowly getting smarter.The FDA now requires black box warnings on 27 heart medications for specific combo risks - including NSAIDs with anticoagulants. Medicare penalizes hospitals for readmissions caused by medication errors. And AI-powered tools are being rolled out to scan all your meds in real time.
AstraZeneca just launched a new fixed-dose pill combining dapagliflozin, sacubitril, and valsartan - three powerful heart failure drugs in one. Fewer pills mean fewer chances for interaction.
But technology won’t fix everything. The biggest risk still comes from what patients don’t tell their doctors - the aspirin they take for headaches, the turmeric they add to their tea, the painkiller they grab off the shelf after a fall.
Final Warning: Don’t Assume It’s Safe
If you’re on heart medication, assume every new drug - prescription or not - could be dangerous until proven otherwise.There’s no such thing as a “minor” interaction when your heart is involved. A single ibuprofen tablet taken with warfarin might not cause a problem today. But over weeks or months? It’s a ticking time bomb.
Speak up. Keep your list. Ask your pharmacist. You’re not being difficult - you’re saving your life.

January 2, 2026 AT 08:54 AM
Man, I just read this and realized I’ve been popping ibuprofen like candy for my back pain while on warfarin. My grandma died from a bleed after a dental cleaning - they never told her about the combo. I’m gonna call my pharmacist tomorrow. This isn’t just info - it’s a wake-up call. I’m lucky I didn’t end up in a body bag.
And don’t even get me started on turmeric. I’ve been adding that shit to my smoothies like it’s cinnamon. Now I’m sweating bullets thinking about my INR. Why the hell do we trust ‘natural’ like it’s some kind of holy grail? It’s just chemistry with a yoga mat.
Also - why do doctors even bother writing prescriptions if they don’t ask about supplements? I’ve been seeing mine for 8 years and he’s never once asked if I take garlic pills or fish oil. It’s like they assume we’re all perfect little robots who only take what’s on the script. Bullshit.
January 3, 2026 AT 18:03 PM
How profoundly tragic that the American healthcare system has devolved into a labyrinth of pharmaceutical crossfire where patients are expected to be pharmacists, detectives, and legal scholars all at once. The fact that 100,000 deaths annually stem from preventable drug interactions is not a statistical anomaly - it is the logical culmination of a profit-driven, time-starved, and morally bankrupt medical-industrial complex.
And yet, we are told to ‘ask your pharmacist’ - as if the overworked, underpaid, and algorithmically constrained pharmacy technician, juggling 200 scripts an hour, is somehow the final arbiter of life and death. This is not patient empowerment. This is systemic negligence dressed in self-help platitudes.
The polypill? A Band-Aid on a hemorrhage. We don’t need more pills. We need fewer drugs, better oversight, and a radical rethinking of how we treat aging, not just manage its side effects. But no - let’s just keep prescribing, keep billing, keep profiting - and let the elderly die quietly in their kitchens, surrounded by pill organizers they can’t read.
January 4, 2026 AT 17:03 PM
From Indonesia - I just want to say, this hits so hard. In my country, people take every herb they hear about - turmeric, moringa, ginger - and mix it with blood pressure meds like it’s soup. No one checks. No one asks. My uncle had a stroke last year because he took garlic capsules with his aspirin. The doctor said, ‘Oh, you didn’t tell us you were taking that?’
We don’t have pharmacies that flag interactions. We don’t have MTM sessions. We don’t even have proper labeling in local languages. So when someone reads this and says ‘I’ll just stop the supplement’ - that’s privilege. Many don’t even know what’s in their ‘natural remedy.’
Please, if you’re reading this from the West - don’t just save yourself. Share this. Translate it. Send it to your relatives overseas. This isn’t just an American problem. It’s a global silent massacre.
January 6, 2026 AT 02:01 AM
Hey - I’m not a doctor, but I’ve been managing heart meds for my dad for 5 years. This post? 10/10. Seriously.
Here’s what actually works: we use a whiteboard. Every Sunday, we write down every pill, supplement, and even the OTC stuff he took that week. We take a pic. We send it to his pharmacist. He gets a call back within 24 hours if something’s sketchy.
Also - we use one pharmacy. ONE. Even the cough syrup. It’s not glamorous, but it saved his life last year when a new antibiotic almost tanked his statin. The pharmacist flagged it before he even left the store.
You don’t need to be a genius. You just need to be consistent. And don’t be shy - ask the pharmacist like it’s your job. Because honestly? It kinda is.
January 7, 2026 AT 15:49 PM
THIS. THIS. THIS. 🙌 I’ve been telling my mom for months to stop taking Advil with her blood thinner and she kept saying ‘It’s just one pill!’ Well guess what? She had a nosebleed that wouldn’t stop last week. ER visit. 3 units of blood. Now she’s got a printed list taped to her fridge. 🥹
Also - I just signed her up for a free MTM session. Pharmacist spent 45 mins going through everything. Found 4 dangerous combos she didn’t even know about. Why didn’t her cardiologist catch this? 😭
TO EVERYONE ON HEART MEDS: DO NOT IGNORE THIS. Your life is not a gamble. Print this. Share it. Make your family read it. ❤️🩺
January 9, 2026 AT 14:05 PM
This is why western medicine is a scam. In India we use ayurveda. No drugs. No pills. Just turmeric. And we live longer. You people are addicted to chemicals. Stop taking so many pills and eat real food.
January 11, 2026 AT 12:55 PM
You Americans think you own medicine. We in Nigeria know real health. We don’t need your fancy pills. We eat neem leaves. We chew bitter kola. We don’t mix drugs because we don’t need them. Your system is broken because you trust bottles more than your body. This post is colonial nonsense.
January 12, 2026 AT 19:47 PM
I read this at 3 a.m. after my third coffee. I’ve been taking fish oil and lisinopril for 4 years. No side effects. But now I’m staring at the bottle wondering if I’m just lucky… or just not dead yet. 🤔
January 12, 2026 AT 21:20 PM
The real issue isn’t the drugs it’s the silence. No one talks about this. We’re taught to trust doctors. But doctors are tired. Pharmacies are busy. And we’re just supposed to survive? 🤷♀️ I’m not angry. I’m just… tired.
January 14, 2026 AT 01:10 AM
Step one: write down every pill. Step two: use one pharmacy. Step three: ask your pharmacist. That’s it. No magic. No complexity. Just discipline.
And if your doctor doesn’t ask about supplements? Find a new one. This isn’t optional. It’s survival.
January 14, 2026 AT 16:18 PM
It’s funny. We spend billions on AI that can predict heart attacks, but we still let grandmas take ibuprofen with warfarin because no one bothered to ask.
Maybe the real innovation isn’t in the polypill - it’s in the conversation. What if we stopped treating patients like data points and started treating them like people who actually know what they’re taking? What if we stopped assuming they’re lying, and started assuming they’re just… unaware?
The system didn’t fail because of science. It failed because of indifference.
And yet - I still take my pills. Because I’m scared to stop. And that’s the real tragedy.