When you’re scheduled for surgery, the last thing you want is for a drug you took years ago to come back and put you in danger. But every year, hundreds of patients experience serious complications because their past drug reactions weren’t properly communicated. It’s not about being forgetful-it’s about not knowing what to say, how to say it, and who needs to hear it.
Why This Matters More Than You Think
A reaction to a drug isn’t just a bad side effect. If you’ve ever had trouble breathing after taking penicillin, broke out in hives after morphine, or went into shock after rocuronium, that’s not a coincidence. That’s a warning sign. The American Society of Anesthesiologists says allergic reactions during anesthesia cause 1.1% of all anesthesia-related deaths. That’s rare-but preventable. In fact, hospitals that use structured communication protocols cut drug-related complications by 37%. That’s not magic. That’s just good process.Here’s the hard truth: if you don’t tell your anesthesiologist about a past reaction, they won’t know to avoid it. And they won’t ask unless you bring it up. Most patients think, “It was years ago,” or “It was just nausea,” or “They’ll check my chart.” But charts get lost. Nurses rush. Doctors assume. You’re the only one who knows your body’s history.
What Counts as a Drug Reaction?
Not everything that feels bad is an allergy. People mix up side effects with true allergic reactions all the time. Here’s how to tell the difference:- Allergy: Immune system response. Symptoms include hives, swelling, wheezing, low blood pressure, anaphylaxis. Happens quickly-minutes to an hour after the drug is given.
- Side effect: Expected, non-immune reaction. Nausea from morphine, dizziness from blood pressure meds, dry mouth from anticholinergics. Not dangerous unless severe.
- Intolerance: Your body handles it poorly. Like severe vomiting after codeine, even if others tolerate it fine.
If you’ve ever needed epinephrine, an IV, or a trip to the ER after a drug, that’s an allergy. If you got sick but didn’t need treatment, it’s still worth mentioning. Anesthesiologists need to know both.
What to Document Before Your Appointment
Don’t wait until the day of surgery. Start at least 72 hours before. Write down:- Drug name: Use the actual name-not “that shot they gave me.” Was it morphine? Ketamine? Succinylcholine? If you don’t know, bring the bottle or a photo of the prescription label.
- Reaction: What happened? “My face swelled,” “I couldn’t breathe,” “I broke out in red bumps,” “My heart raced.” Be specific.
- Timing: How soon after the drug was given? Within 5 minutes? 30 minutes? 2 hours?
- Treatment: Did you get antihistamines? Steroids? Epinephrine? Were you hospitalized?
- Other drugs you take: Even vitamins, herbal supplements, and over-the-counter painkillers. Some herbs like St. John’s Wort can interfere with anesthesia.
Pro tip: If you’ve had a serious reaction, ask your doctor for a drug allergy card. Many allergists give these out. It’s a small plastic card you can keep in your wallet. It says: “Allergic to [drug]. Avoid all related drugs. Contact [doctor].”
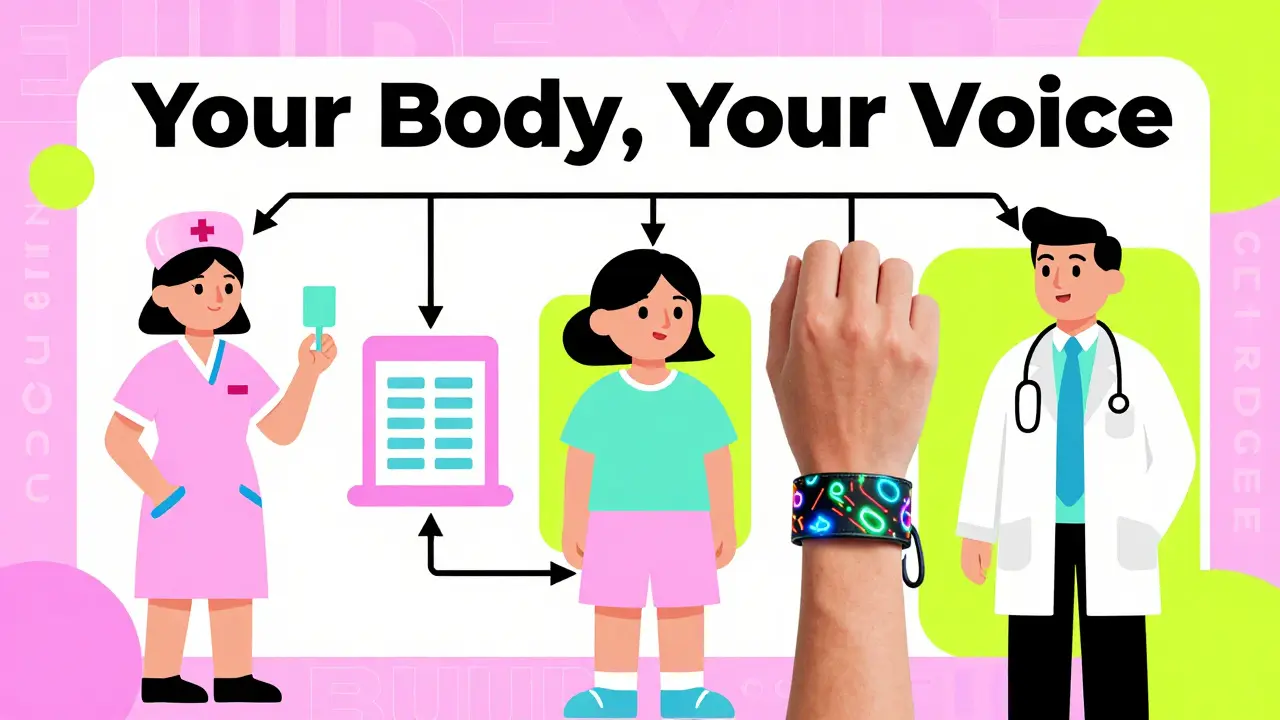
Who You Need to Tell-And When
It’s not enough to tell one person. You need to tell everyone involved:- Your primary doctor: Tell them as soon as you know you’re having surgery. They’ll send a note to the surgical team.
- The pre-op nurse: They’ll ask you questions. Don’t just say “I’m allergic to penicillin.” Say: “I had a rash and swelling after penicillin in 2019. I was treated with Benadryl and steroids.”
- The anesthesiologist: This is the most important person. They decide what drugs go into your body. They will review your history. If they’re unsure, they might delay surgery to consult an allergist.
- The pharmacist: Hospitals now have pharmacists who screen your chart 24 hours before surgery. They look for interactions and allergies. Make sure they’re aware.
Don’t assume your chart says it all. In a 2022 study, 32% of patients couldn’t remember the exact drug name. But 87% of allergists recommend patients carry their own allergy info. Don’t rely on memory. Bring it written down.
What If You Can’t Remember the Drug Name?
This happens more than you think. You might say, “I had a bad reaction to something they gave me for my wisdom teeth.” That’s not enough.Here’s how to figure it out:
- Check old medical records. Request them from your dentist or doctor. Most offices keep records for 7+ years.
- Look at old prescriptions. Did you get a new bottle after the reaction? The label might say the drug.
- Ask family. Did someone else go with you? Did they remember the name?
- Use a drug identification app. Apps like WebMD Pill Identifier let you upload a photo of a pill and find the name.
If you truly can’t find out, say: “I had a severe reaction to an IV drug during a dental procedure around 2018. I had swelling and trouble breathing. I don’t know the name, but I need to avoid anything similar.” That’s enough for them to proceed with caution.
High-Risk Drugs to Watch Out For
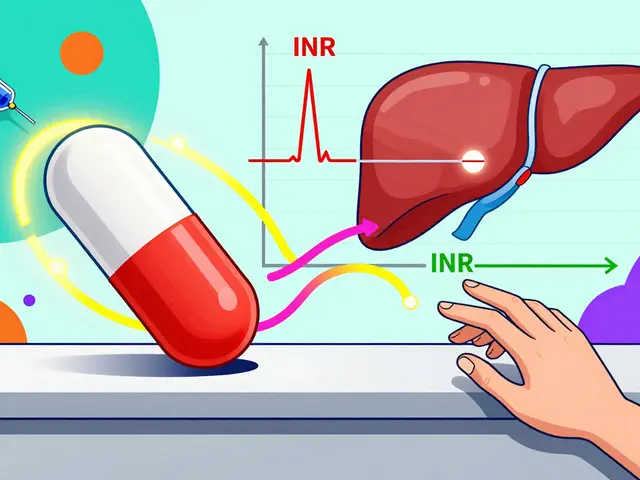
Some drugs are more likely to cause reactions. If you’ve had any reaction, avoid these unless cleared by an allergist:- Neuromuscular blockers: Rocuronium, succinylcholine, vecuronium-common in anesthesia. Responsible for 60% of anaphylaxis cases during surgery.
- Antibiotics: Penicillin, cephalosporins, vancomycin. Penicillin allergies are the most common.
- Opioids: Morphine, codeine, fentanyl. Can cause histamine release, mimicking allergy.
- Latex: Not a drug, but a common allergen in gloves, tubing, and IV bags. Many hospitals now use latex-free supplies, but you still need to say if you’re allergic.
- MAO inhibitors: Used for depression. Must be stopped 2 weeks before surgery. Can cause deadly spikes in blood pressure with certain anesthetics.
If you’ve had a reaction to one drug in a class, you might react to others. For example, if you’re allergic to penicillin, you might also react to amoxicillin or ampicillin. Your anesthesiologist will need to know the full family.
What Happens If You Don’t Say Anything?
A 2021 incident reported to the Anesthesia Patient Safety Foundation involved a patient with a known vancomycin allergy. The chart had it listed-but the anesthesiologist didn’t see it because it was buried in a note. The patient went into anaphylaxis mid-surgery. They survived, but spent 10 days in ICU.Another case: a woman told her nurse she was allergic to “pain meds.” She meant codeine. The team gave her morphine. She vomited violently for hours after surgery. She didn’t have an allergy-just intolerance. But because she didn’t clarify, they assumed the worst and gave her a stronger drug.
These aren’t rare. They happen because communication breaks down. You’re the only one who can prevent that.
What If You’re Having Emergency Surgery?
In emergencies, there’s no time for long conversations. But you still need to act:- Wear a medical alert bracelet. If you’ve had a serious reaction, get one. It says “Allergic to [drug]” and “See wallet card.”
- Tell the EMTs or ER staff as soon as you arrive. Don’t wait for them to ask.
- If you’re unconscious, have someone you trust carry your allergy card.
Even in emergencies, 37% of hospitals still have incomplete allergy records. Your card could save your life.
What Comes After Surgery?
If you had a reaction during or after surgery, even if it was mild, you need follow-up:- Ask for a referral to an allergist. They can test you to confirm what you’re allergic to.
- Get a written report. It should list the drug, reaction, and which drugs to avoid.
- Update your EHR. Make sure your primary doctor, surgeon, and pharmacy have the updated info.
- Carry your allergy card. Update it every year.
Stanford’s guidelines say: if you’re still unsure what caused the reaction, you should only get anesthesia again for emergencies until you’ve been tested. That’s not fear-it’s safety.
Final Checklist Before Surgery
Use this before your pre-op visit:- Write down every drug you’ve ever reacted to-name, reaction, date.
- Bring your current medication list, including vitamins and herbs.
- Print or carry your allergy card.
- Ask your doctor for a copy of your medical records from past reactions.
- Confirm with the hospital that your allergy is in their system.
- Repeat your reaction details to the anesthesiologist-out loud, in your own words.
It’s not about being difficult. It’s about being the expert on your own body. No one else has the full picture. And if you don’t speak up, someone might make a deadly assumption.
What if I think I’m allergic but I’m not sure?
Always report it. Even if it turned out to be a side effect, your anesthesiologist needs to know. They can choose safer alternatives. It’s better to be cautious than to risk a real reaction. Many patients say they’re “allergic” when they had nausea or dizziness-but that still matters. It tells the team your body reacts poorly to certain drugs.
Can I just tell the nurse and forget about it?
No. Nurses are busy. Charts get updated by multiple people. You need to tell your anesthesiologist directly. Ask to speak with them before surgery. Say: “I had a serious reaction to [drug] and want to make sure it’s on your radar.” Don’t assume it’s already recorded.
Do I need to tell them about my marijuana or alcohol use?
Yes. Substance use affects how your body handles anesthesia. Regular alcohol use can make you resistant to sedatives. Marijuana can lower blood pressure and interact with pain meds. Being honest helps them dose safely. They’re not judging-they’re protecting you.
What if I had a reaction as a child? Does it still matter?
Yes. Allergies don’t always go away. A reaction to penicillin at age 8 might still be active at 40. Some people outgrow them, but you won’t know unless you’re tested. Until then, assume it’s still a risk.
Can I get tested after surgery to confirm my allergy?
Yes. Allergists can do skin tests or blood tests to confirm drug allergies. The Spanish Journal of Anesthesia recommends testing within 4-8 weeks after a reaction. This helps you avoid unnecessary restrictions in the future. Don’t wait-schedule it.