When you’re 70, your body doesn’t process medicine the same way it did at 40. That’s not just a guess-it’s science. A 75-year-old taking the same dose of a blood pressure pill as a 50-year-old might end up dizzy, confused, or even hospitalized. This isn’t rare. In fact, medication dosage adjustments for aging bodies and organs are one of the most critical, yet overlooked, parts of senior healthcare. About 35% of hospital visits among people over 65 are caused by bad reactions to medicines, not the disease itself. And most of those reactions happen because the dose never changed as the body changed.
Why Aging Changes How Drugs Work
Your body doesn’t just slow down with age-it rewires how drugs move through it. Think of it like a highway system that’s gotten narrower, slower, and full of detours. Four key changes happen:- Absorption: Stomach acid drops by 20-30%, and blood flow to the gut slows. That means pills dissolve slower, and your body takes in less of the drug.
- Distribution: You lose muscle and gain fat. Since many drugs bind to fat, they linger longer in your body. Water-soluble drugs, like some diuretics, become more concentrated because you have less water overall.
- Metabolism: Your liver shrinks and gets less blood flow. It can’t break down drugs as fast. For many medications, liver clearance drops by 30-50% after 65.
- Excretion: Kidneys filter blood slower. After age 30, your kidney function drops about 8 mL per minute every decade. By 70, many people have less than half the kidney function they had in their 30s.
These changes mean a drug that was perfectly safe at 50 can become dangerous at 75. A standard 300 mg dose of gabapentin for nerve pain? That’s too much. A 100-150 mg dose is safer. Metformin for diabetes? It’s often stopped if kidney function falls below 30 mL/min. These aren’t opinions-they’re guidelines backed by decades of research.
The ‘Start Low, Go Slow’ Rule
This isn’t just a saying. It’s the golden rule of geriatric prescribing. The American Geriatrics Society has pushed this approach since the 1980s. It means starting at 25-50% of the usual adult dose and increasing it slowly, only if needed.Take warfarin, a blood thinner. Older adults often need 20-30% less than younger patients. Too much? Risk of internal bleeding. Too little? Risk of stroke. The same goes for antidepressants, sleep aids, and even painkillers. A 2020 study found that 27% of nursing home drug reactions were due to doses that were never adjusted for age.
Doctors don’t always know this. A 2021 survey found 65% of U.S. physicians feel undertrained in geriatric dosing. That’s why many seniors end up on the same pills they took at 50-long after their body stopped handling them the same way.
How to Calculate the Right Dose
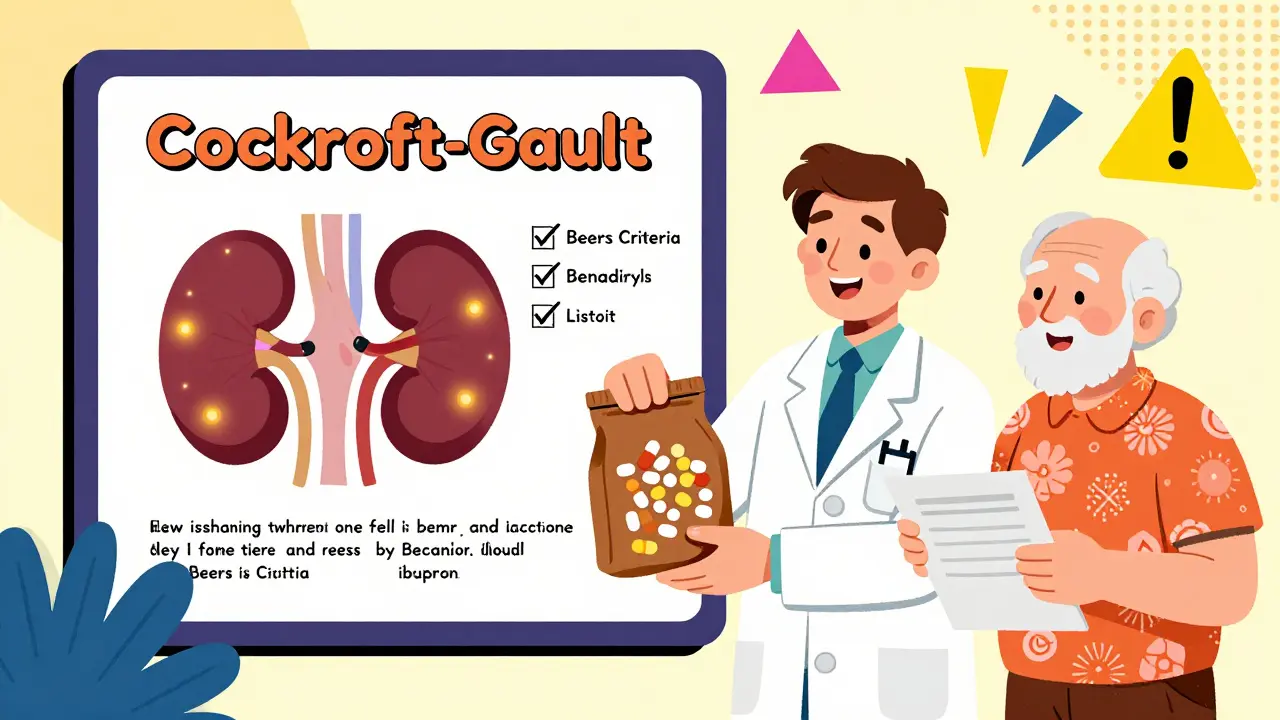
There’s no one-size-fits-all formula, but two tools are used in clinics every day:- Cockcroft-Gault Equation: This calculates kidney function using age, weight, and a blood test for creatinine. For men: [(140 - age) × weight in kg] / (72 × serum creatinine). For women, multiply the result by 0.85. If the result is below 50 mL/min, most kidney-cleared drugs need a lower dose.
- Child-Pugh Score: Used for liver problems. It looks at bilirubin, albumin, and other markers. A score of 7-9 means cut the dose in half. A score of 10-15? Avoid the drug entirely.
For drugs like digoxin, doctors use therapeutic drug monitoring-measuring the exact level in the blood. In seniors, the safe range is 0.5-0.9 ng/mL. In younger people, it’s 0.8-2.0. That’s a huge difference. But here’s the problem: only 15% of commonly prescribed drugs have this kind of blood test available.
High-Risk Medications for Seniors
The 2023 Beers Criteria® lists 30 types of drugs that are risky for older adults. Some are obvious. Others aren’t.- Benzodiazepines (like diazepam): Increase fall risk by 50%. Often prescribed for anxiety or sleep, but they make you unsteady.
- NSAIDs (like ibuprofen): Raise the chance of stomach bleeding by 300%. Even a daily aspirin can be dangerous if you’re on blood thinners.
- Anticholinergics (like diphenhydramine in sleep aids): Double dementia risk with long-term use. Found in many over-the-counter cold and allergy pills.
- Antipsychotics (used for behavior in dementia): Increase stroke risk and death. Often overused in nursing homes.
Many seniors take these without realizing they’re high-risk. A 78-year-old woman might take Benadryl for allergies, melatonin for sleep, and ibuprofen for arthritis-all on the Beers list. That’s three red flags in one pill bottle.
Polypharmacy: The Silent Killer
More than half of seniors take five or more prescription drugs. That’s called polypharmacy. It’s not always bad-some people need multiple meds. But the more drugs you take, the higher the chance of bad interactions and wrong doses.Imagine someone on warfarin, lisinopril, metformin, simvastatin, and gabapentin. Each one needs its own adjustment. Warfarin needs blood tests. Metformin needs kidney checks. Gabapentin needs dose reduction. If one doctor prescribes each drug without talking to the others, mistakes happen.
Pharmacists cut medication errors by 67% in geriatric patients when they’re involved in dosing decisions. That’s why programs like the University of North Carolina’s “Pharm400” use weekly blister packs and weekly check-ins. Their results? A 22% drop in hospital visits.
What You Can Do
You don’t need to be a doctor to protect yourself or a loved one. Here’s what actually works:- Do a brown bag review: Every 6 months, bring all your pills-prescription, OTC, supplements-to your doctor or pharmacist. Don’t just list them. Show them the bottles.
- Ask: “Is this still needed?” Especially for drugs taken for years. Many are never re-evaluated.
- Check kidney and liver function yearly: A simple blood test can tell if your dose needs changing.
- Use pill organizers: They help avoid double-dosing or skipping pills.
- Involve a family member: Studies show caregiver involvement improves adherence by 37%.
Electronic health records now have alerts for kidney dosing. But they’re only as good as the data entered. If your creatinine level isn’t updated, the alert won’t trigger. That’s why your input matters.
The Future of Geriatric Dosing
The field is changing fast. The FDA now requires age-specific data in clinical trials. The American Geriatrics Society is adding frailty scores and walking speed to dosing guidelines-not just age. AI tools like MedAware are being tested to predict dangerous doses before they’re prescribed.But the biggest shift? Moving away from “chronological age” to “functional age.” A 75-year-old who walks fast, thinks clearly, and has strong kidneys might need a full dose. A 68-year-old with slow walking speed, memory issues, and low kidney function might need a quarter of the standard dose. That’s the future.
By 2030, experts predict 70% of high-risk medications will be dosed using individualized pharmacokinetic models. That means blood tests, kidney numbers, and even cognitive scores will guide each pill. It’s not science fiction-it’s coming.
For now, the best tool you have is awareness. Ask questions. Demand reviews. Don’t assume a prescription is safe just because it’s been taken for years. Your body isn’t the same as it was. Your meds shouldn’t be either.
Why do older adults need lower medication doses?
Older adults need lower doses because their bodies change with age: kidneys filter slower, liver breaks down drugs less efficiently, body fat increases while muscle decreases, and stomach acid drops. These changes mean drugs stay in the system longer and can build up to toxic levels if the dose isn’t adjusted. A standard adult dose can become dangerous for someone over 65.
What is the Cockcroft-Gault equation used for?
The Cockcroft-Gault equation estimates kidney function (creatinine clearance) using age, weight, and blood creatinine levels. It helps doctors decide if a drug dose needs to be lowered for seniors. If the result is below 50 mL/min, many medications-especially those cleared by the kidneys-must be reduced to avoid toxicity.
Which medications are most dangerous for seniors?
According to the 2023 Beers Criteria®, high-risk drugs include benzodiazepines (increase fall risk by 50%), NSAIDs like ibuprofen (triple gastrointestinal bleeding risk), anticholinergics (double dementia risk), and antipsychotics (increase stroke risk). Even common OTC meds like diphenhydramine (Benadryl) can be harmful with long-term use.
How can I tell if my medication dose is too high?
Signs include dizziness, confusion, memory lapses, falls, extreme fatigue, nausea, or sudden changes in mood or behavior. These often appear after a new prescription or dose increase. If you notice these, don’t stop the drug-talk to your doctor or pharmacist. A simple blood test or kidney function check can confirm if the dose is too high.
Should I stop taking a medication if I’m worried about side effects?
Never stop a prescribed medication on your own. Some drugs, like blood pressure or heart meds, can cause serious rebound effects if stopped suddenly. Instead, schedule a medication review with your doctor or pharmacist. Bring all your pills in a bag. They can help determine if the drug is still necessary, if the dose can be lowered, or if a safer alternative exists.
Can pharmacists help with medication dosing for seniors?
Yes-pharmacists reduce medication errors in older adults by 67% when they’re involved in care. They check for drug interactions, adjust doses based on kidney or liver function, spot high-risk medications, and help simplify regimens. Many hospitals and clinics now have geriatric pharmacists on staff specifically for this purpose. Ask your doctor to refer you.
What to Do Next
If you or someone you care for is over 65 and taking multiple medications:- Set up a brown bag review within the next 30 days.
- Ask for a recent creatinine blood test if it hasn’t been done in the last year.
- Check the Beers Criteria® list online-see if any of your meds are flagged.
- Request a pharmacist consultation through your doctor’s office or pharmacy.
Medication safety isn’t about cutting pills in half. It’s about matching the dose to the body you have now-not the one you had 20 years ago. That’s the difference between staying healthy and ending up in the hospital.


January 16, 2026 AT 21:04 PM
Bro, I saw my grandma on 12 meds last week and she’s fine. Why are we overcomplicating this? My uncle died from a stroke and he was on like three pills. You’re acting like every old person is one typo away from dying. Chill.
January 17, 2026 AT 04:53 AM
Let’s be real-this whole post is just pharmaceutical industry fearmongering dressed up as ‘science.’ The FDA and Big Pharma want you scared so you’ll keep taking drugs they’ve barely tested on seniors. They don’t care if you live or die-they care if your prescription refills keep coming. Wake up.
January 17, 2026 AT 06:22 AM
The Cockcroft-Gault equation is outdated and statistically flawed when applied to frail elderly populations with low muscle mass. Creatinine-based estimations systematically overestimate GFR in older adults due to reduced muscle mass, leading to inappropriate dose escalation. This is why the CKD-EPI equation is now preferred in geriatric pharmacology-yet 78% of primary care EMRs still default to Cockcroft-Gault because it’s easier to code. This isn’t just negligence-it’s systemic epistemic failure.
January 17, 2026 AT 18:31 PM
I’m a nurse and this is spot on. I’ve seen so many seniors on Benadryl for sleep and then fall in the bathroom. Their families don’t even realize it’s the meds. Please, if you’re reading this-ask your pharmacist. They’re the real heroes here.
January 18, 2026 AT 11:37 AM
Yessss!! 🙌 My abuela was on 14 meds until I did the brown bag thing. Cut her down to 5. She’s walking again. 🌿💊 #MedicationAudit #GrandmaWins
January 19, 2026 AT 21:31 PM
Look, I get it-your body changes. But here’s the thing: in India, we don’t have fancy labs or pharmacists checking creatinine every month. We have grandmas taking pills their son brought from the U.S. and doctors who prescribe by habit. This post is brilliant, but it’s written for people who have access to care. What about the 80% who don’t? We need simpler, global guidelines-not just jargon for the privileged.
January 20, 2026 AT 10:57 AM
My dad turned 72 last year and we started doing monthly med reviews. He was on gabapentin for ‘nerve pain’-never had nerve pain. Turns out it was just arthritis. We swapped it for a topical cream. He’s sleeping better, no dizziness. It’s not rocket science. Just care. And asking questions. You don’t need a PhD to save your own life.
January 21, 2026 AT 16:01 PM
This isn’t just about medicine-it’s about respect. We treat older people like broken machines that need tuning, not like humans who’ve lived decades and deserve to be heard. If your doctor won’t listen when you say ‘I feel weird,’ find a new one. Your body is telling you something. Listen. Fight for your health. You’re not too old to demand better.
January 23, 2026 AT 03:02 AM
Regarding the Beers Criteria®: the use of the registered trademark symbol is mandatory in formal publications, yet it is frequently omitted in online forums, which undermines the credibility of the source. Additionally, the term ‘polypharmacy’ is often misused-it refers specifically to the use of five or more medications, not merely multiple medications. Precision matters.
January 25, 2026 AT 01:40 AM
My mom’s on warfarin. They never told us to check INR every 2 weeks. She almost bled out. Don’t assume they know. Ask. Always.
January 26, 2026 AT 14:49 PM
Why are we letting foreigners tell us how to treat our own elders? This is American medicine. We don’t need some WHO pamphlet telling us to cut doses. We’re the best in the world.
January 28, 2026 AT 08:36 AM
They’re coming for your pills next. First they say ‘lower the dose,’ then they say ‘stop the pill,’ then they say ‘you don’t need it.’ This is the beginning of government-controlled medicine. They’ll decide what you can take. Wake up. This isn’t science-it’s control.
January 28, 2026 AT 09:58 AM
According to the CDC, 89% of medication errors in seniors occur due to transcription errors in EHRs. Yet this post blames ‘doctors not knowing.’ That’s misleading. The real problem? EHRs that auto-populate old doses. The software is broken. Not the doctors. Fix the system, not the people.
January 29, 2026 AT 14:06 PM
Did you know the FDA approved 87% of geriatric drugs without any trials on patients over 75? The data is fabricated. The whole system is rigged. They use ‘clinical guidelines’ to cover up the fact that they never tested it. You’re being used as a lab rat.
January 30, 2026 AT 20:10 PM
I’ve been taking metformin for 15 years. My kidneys are fine. Why should I change anything? You’re making old people paranoid. If it ain’t broke, don’t fix it.
February 1, 2026 AT 05:59 AM
My husband died because they gave him too much blood thinner. They said ‘it’s standard.’ Standard? Standard doesn’t mean safe. Now I’m screaming into the void. No one listens. No one cares.
February 3, 2026 AT 04:20 AM
They don’t want you to know this. The real reason doses are too high? Because if they lowered them, drug companies would lose billions. That’s why they fund the ‘guidelines.’ It’s all money. You’re a product. Your body? Just a revenue stream.
February 4, 2026 AT 20:34 PM
My 78-year-old neighbor takes a quarter of her pill every day. She’s been doing it for years. No doctor ever told her to. She’s fine. Sometimes, the body knows.
February 5, 2026 AT 04:00 AM
My mom’s 71, walks 5 miles a day, hikes mountains, and reads three books a week. Her kidneys are better than mine. She takes full dose. Age isn’t the problem-function is. Let’s stop treating 70 like a disease.
February 6, 2026 AT 06:42 AM
It is imperative to underscore the ethical obligation incumbent upon healthcare practitioners to individualize pharmacotherapy in geriatric populations. The principles of beneficence and nonmaleficence necessitate a recalibration of dosing regimens predicated upon physiological, not chronological, parameters. The integration of functional assessments, including gait speed and cognitive screening, into clinical decision-making protocols represents not merely an advancement, but a moral imperative.