OTC Drug Interaction Checker
Check Your Medications
Enter your current medications to see if they interact dangerously with common OTC drugs.
Results
When a medication moves from prescription-only to over-the-counter (OTC), it sounds like good news: easier access, lower cost, and more control over your health. But behind that convenience lies a hidden risk many consumers don’t see coming. OTC drugs aren’t harmless - they’re still powerful chemicals that can cause serious harm if used incorrectly. Every time a drug makes the switch from prescription to OTC, millions of people suddenly start using it without ever talking to a doctor. And that’s where problems begin.
What Happens When a Drug Goes OTC?
A prescription drug becomes OTC only after years of safety reviews by regulators like the U.S. Food and Drug Administration (FDA). The goal isn’t just to make drugs cheaper - it’s to give people access to treatments they can safely manage on their own. For example, ibuprofen was once prescription-only. After studies showed it was safe for short-term use in healthy adults, it switched to OTC in 1984. The price dropped from $30-$40 a month to $5-$10. That’s a win for consumers.
But here’s the catch: when a drug goes OTC, it doesn’t just become more available - it becomes more widely used. People who never would’ve taken it with a doctor’s oversight now grab it off the shelf. Someone with undiagnosed high blood pressure buys pseudoephedrine for a stuffy nose. A person on blood thinners starts taking aspirin for headaches. These aren’t rare mistakes. They’re common.
The Hidden Dangers of Self-Medication
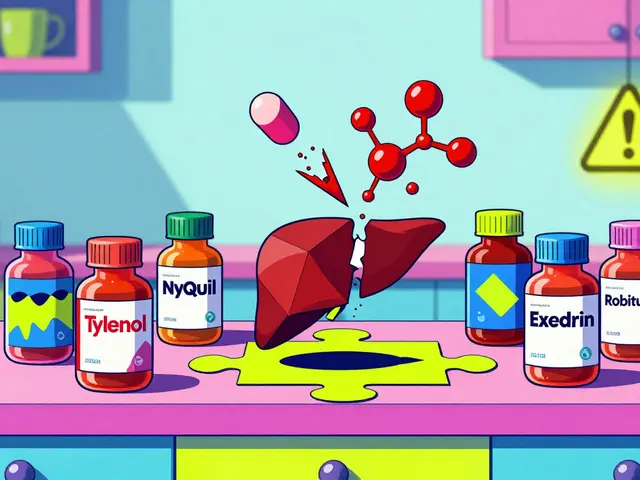
OTC drugs are designed for short-term, mild symptoms. But many people use them for weeks or months without realizing the risks. Take acetaminophen (Tylenol). It’s in more than 600 OTC products - cold medicines, sleep aids, pain relievers. People don’t realize they’re doubling up. A Reddit user named PharmTech2020 described seeing patients take double doses because they didn’t know both their painkiller and cold tablet contained acetaminophen. Liver damage from too much acetaminophen is one of the top reasons people end up in emergency rooms.
NSAIDs like ibuprofen and naproxen are another silent threat. They’re great for a headache or sore muscle. But long-term use? That’s where things get dangerous. Studies show prolonged NSAID use can cause stomach ulcers, kidney failure, and even heart attacks - especially in older adults or those with existing conditions. And without a doctor monitoring them, people have no idea they’re at risk.
Even something as simple as an antihistamine like diphenhydramine (Benadryl) can be risky. The American Geriatrics Society lists it as one of 30 OTC drugs that should be avoided by adults over 65. Why? It can cause confusion, dizziness, and falls. Older people often take it for sleep - not realizing it’s not a sleep aid, it’s an allergy medicine with serious side effects in aging bodies.
Drug Interactions You Never Saw Coming
One of the biggest dangers of OTC drugs is how they interact with other medications. A 2023 study from Bangalore found that 77% of patients had no idea about drug contraindications. That means they didn’t know, for example, that taking a decongestant like pseudoephedrine while on an MAOI antidepressant could cause a sudden, dangerous spike in blood pressure. Or that mixing sleep aids with prescription sedatives could slow breathing to dangerous levels.
The FDA warns that even mild interactions can cause real harm. Alcohol with antihistamines? Drowsiness turns into dangerous dizziness. Aspirin with blood thinners? Risk of internal bleeding skyrockets. And here’s the kicker: most people don’t tell their doctor what OTC drugs they’re taking. They think it’s not “real medicine.” Dr. David Kaelber from Case Western Reserve University says, “The biggest risk with OTC medications is that people don’t realize they’re taking a medication.”

Who’s Most at Risk?
Not everyone is equally vulnerable. The biggest danger zones are:
- Older adults - Their bodies process drugs slower. They often take 5+ medications. The Beers Criteria lists 30 OTC drugs that are risky for people over 65.
- People with chronic conditions - Diabetes, heart disease, kidney problems, liver disease - these all change how your body handles OTC drugs. NSAIDs can wreck kidneys in people with diabetes. Decongestants can spike blood pressure in those with hypertension.
- Those taking multiple drugs - If you’re on three or more prescriptions, the chance of a bad interaction jumps dramatically. A 2022 survey found only 32% of OTC users consistently read labels. That’s a recipe for disaster.
- Children - Dosing errors are common. A child’s weight matters more than age. Many parents give adult doses because “it’s just a pill.”
How to Use OTC Drugs Safely
Just because a drug is OTC doesn’t mean it’s risk-free. Follow these steps before taking anything:
- Read the Drug Facts label - Not the fancy packaging. Look for the small print on the back. It lists active ingredients, warnings, and directions. If you don’t understand it, don’t take it.
- Check for duplicate ingredients - If you’re taking two products, make sure they don’t have the same active ingredient. Acetaminophen, ibuprofen, and antihistamines are the most common culprits.
- Ask a pharmacist - Pharmacists aren’t just there to hand you the box. They’re trained to spot interactions. Tell them what prescriptions you’re on, what supplements you take, and what symptoms you’re treating. Many pharmacies now offer free medication reviews.
- Know your limits - If a symptom lasts more than a few days, get checked out. OTC drugs are for temporary relief, not long-term fixes. Persistent pain, fatigue, or congestion could be signs of something serious.

What’s Changing in 2026?
The FDA is trying to make OTC labels easier to understand. New labels now use larger fonts, clearer headings, and simpler language. Some companies are adding QR codes that link to safety videos or interactive interaction checkers. Walmart started testing this in 2023 - scanning a code on a pain reliever can show you if it’s safe to take with your blood pressure med.
But technology won’t fix everything. The real problem is awareness. A 2023 study found that 85% of patients in India trusted pharmacists - but only 13% knew about adverse drug effects. That’s not trust - that’s ignorance. And it’s dangerous.
Final Thought: OTC Doesn’t Mean Risk-Free
OTC switches save money and improve access. But they also shift responsibility - from doctors to you. You’re now the gatekeeper of your own health. That’s empowering - but only if you know what you’re doing.
Every pill you take, whether prescription or OTC, has a job to do. And if you don’t understand how it works - or what it might do to your body - you’re playing with fire. The safest OTC drug is the one you never take without thinking. Ask questions. Read labels. Talk to your pharmacist. And if something doesn’t feel right? See a doctor. No OTC pill is worth ignoring a real problem.
Can OTC drugs really cause serious harm?
Yes. While OTC drugs are generally safe when used as directed, misuse - like taking too much, combining them with other drugs, or using them long-term - can lead to liver damage, kidney failure, internal bleeding, heart attacks, and even death. Acetaminophen overdose is the leading cause of acute liver failure in the U.S. NSAIDs can cause stomach ulcers and kidney damage in people with underlying conditions. The risks are real, even if the drugs are sold on store shelves.
Why do some drugs switch from prescription to OTC?
Regulators approve OTC switches only after years of data proving the drug is safe for self-use. The condition must be easy to self-diagnose (like heartburn or minor pain), the drug must have a wide safety margin, and users must be able to follow label instructions correctly. The goal is to reduce healthcare costs and improve access - but safety always comes first. For example, famotidine (Pepcid) switched to OTC after studies showed it was safe for occasional heartburn without medical supervision.
Are OTC drugs safer than prescription drugs?
Not necessarily. Prescription drugs are monitored by doctors, who check for interactions, adjust doses, and watch for side effects. OTC drugs remove that safety net. A drug that’s safe under supervision can become dangerous without it. The difference isn’t in the drug - it’s in the oversight. A prescription drug isn’t “stronger” - it’s just used with more caution.
What should I do if I’m taking multiple medications?
If you take three or more medications - prescription or OTC - you’re at high risk for harmful interactions. Always consult a pharmacist before adding any new OTC product. Bring a list of everything you take, including supplements and herbal remedies. Many pharmacies offer free medication reviews. Don’t assume OTC means safe - especially if you have conditions like high blood pressure, diabetes, or kidney disease.
How can I tell if an OTC drug is right for me?
Start by reading the Drug Facts label. Look for the “Warnings” section - it will tell you if you should avoid the drug based on your health conditions. Check if the active ingredient is already in another medicine you’re taking. If you’re unsure, ask a pharmacist. And if your symptoms don’t improve in 3-5 days, see a doctor. OTC drugs are for short-term relief - not long-term management.