Many people carry a label in their medical record: sulfa allergy. It sounds simple. But what it actually means-and what you should avoid-is far more complicated than most doctors and patients realize. If you’ve ever been told you can’t take a diuretic, a diabetes pill, or even a pain reliever because you’re allergic to sulfa, you might be unnecessarily avoiding safe, effective medications. The truth? Most people who think they have a sulfa allergy don’t actually have one-and even if they do, it likely doesn’t apply to most drugs with sulfonamide in the name.
What Is a Real Sulfa Allergy?
The term sulfa allergy usually refers to an allergic reaction to sulfonamide antibiotics-drugs like sulfamethoxazole (in Bactrim), sulfadiazine, or sulfacetamide. These were among the first antibiotics ever developed, introduced in the 1930s. Back then, reactions were more common because doses were higher and monitoring was minimal. Today, true IgE-mediated allergic reactions to these antibiotics occur in only 0.3% to 0.5% of the population, according to the American Academy of Allergy, Asthma & Immunology. Yet, up to 12% of people say they’re allergic. That’s a huge gap.Most of those reports aren’t true allergies at all. They’re rashes that came on days after starting the antibiotic-common with many drugs-or nausea, headaches, or dizziness. These are side effects, not immune responses. Even a mild skin rash from sulfamethoxazole doesn’t mean you’ll react to every other sulfonamide-containing drug. And yet, that label sticks. For years. Decades.
The Big Misunderstanding: Not All Sulfonamides Are the Same
Here’s the key point most people miss: not all drugs with "sulfonamide" in the name are the same. Chemically, they all have an SO₂NH₂ group. But that’s like saying all cars have wheels-doesn’t mean a bicycle and a truck are the same.Antibiotic sulfonamides have two specific chemical features that trigger allergic reactions: an arylamine group at the N4 position and a nitrogen-containing ring at the N1 position. These structures create reactive metabolites that bind to proteins in your body, forming what your immune system sees as a threat. Nonantimicrobial sulfonamides? They lack these exact pieces. Celecoxib (Celebrex), hydrochlorothiazide (HCTZ), furosemide (Lasix), and acetazolamide (Diamox) all contain the sulfonamide group-but none have the N4-arylamine. That’s why your immune system doesn’t recognize them the same way.
Studies show this clearly. A 2022 review of over 10,000 patients found that those with a history of sulfonamide antibiotic allergy had a reaction risk to nonantimicrobial sulfonamides of just 1.3%-almost identical to the 1.1% risk in people with no such history. That’s not a meaningful difference. It’s like saying someone allergic to peanuts might react to almonds. It’s possible, but it’s not because they’re related. It’s because of coincidence or another factor.
What You Can Likely Take (Even With a Sulfa Allergy)
If you’ve been told to avoid all "sulfa" drugs, here’s what you can probably still use safely:- Hydrochlorothiazide (HCTZ) - a common blood pressure pill
- Furosemide (Lasix) - a water pill used for heart failure or swelling
- Celecoxib (Celebrex) - a COX-2 inhibitor for arthritis pain
- Acetazolamide (Diamox) - used for glaucoma, altitude sickness, or seizures
- Metformin - yes, even though it’s sometimes confused with sulfa, it’s not a sulfonamide at all
These drugs are not just safe-they’re often the best or only option for managing conditions like hypertension, heart failure, or glaucoma. Avoiding them because of a mislabeled allergy can lead to worse outcomes. For example, patients with a "sulfa allergy" label are 2.4 times more likely to get fluoroquinolones like ciprofloxacin instead of the right antibiotic. But fluoroquinolones carry black box warnings for tendon rupture, nerve damage, and aortic aneurysm. Is that really safer?
What You Should Still Avoid
There are exceptions. One big one: dapsone. It’s used for leprosy, certain skin conditions, and Pneumocystis pneumonia (PCP) prevention in people with HIV. Dapsone shares structural similarities with antibiotic sulfonamides-including the N4-arylamine group. Studies show a 13% reaction rate in people with prior sulfonamide antibiotic allergies. So if you’ve had a severe reaction like Stevens-Johnson syndrome to sulfamethoxazole, dapsone should be approached with caution.Also avoid any other antibiotic sulfonamide: sulfadiazine, sulfisoxazole, sulfacetamide (eye drops), and sulfasalazine (used for ulcerative colitis and rheumatoid arthritis). Sulfasalazine is tricky-it breaks down into sulfapyridine (an antibiotic sulfonamide) and 5-ASA. So if you’re allergic to sulfonamide antibiotics, you may react to sulfasalazine too.
Why This Matters Beyond Your Prescription
This isn’t just about avoiding a rash. It’s about antibiotic resistance. When doctors can’t use sulfamethoxazole-trimethoprim because of a mislabeled allergy, they turn to broader-spectrum drugs like vancomycin, linezolid, or carbapenems. These are powerful antibiotics meant for life-threatening infections. Overusing them pushes bacteria to evolve resistance faster. The CDC estimates that inappropriate antibiotic choices due to false sulfa allergy labels increase resistance rates in E. coli by 8.3% and Staphylococcus aureus by 12.7%.And it’s expensive. In the U.S. alone, this mislabeling costs the healthcare system an estimated $1.2 billion a year in extra drug costs, longer hospital stays, and unnecessary tests. That’s money spent because of confusion, not science.
What Should You Do If You Think You Have a Sulfa Allergy?
Step one: Look at your records. What exactly happened? Did you get a rash five days after taking Bactrim? That’s not an allergy-it’s a common side effect. Did you break out in hives 20 minutes after the first dose? That’s a red flag. Did you have trouble breathing or swelling of the face? That’s a true anaphylactic reaction-and you should avoid all antibiotic sulfonamides.Step two: Ask for a review. Talk to your doctor or an allergist. Many clinics now offer "de-labeling" programs. For low-risk reactions (like a delayed rash), an outpatient oral challenge with a nonantimicrobial sulfonamide like hydrochlorothiazide is safe and effective. Studies show a 99.2% success rate. For higher-risk cases (anaphylaxis, SJS), skin testing or a supervised graded challenge can confirm whether you’re truly allergic.
Step three: Update your records. If testing shows you’re not allergic, ask your doctor to change "sulfa allergy" to "no true sulfa allergy" or "reaction to sulfamethoxazole in 2010, no cross-reactivity expected." This helps future providers make better decisions.
Don’t Confuse Sulfonamide With Sulfate, Sulfite, or Sulfur
This is a common and dangerous mix-up. Many people think "sulfa allergy" means they can’t take anything with "sulf" in the name. That’s wrong.- Sulfates (like magnesium sulfate or heparin) - no connection
- Sulfites (in wine, dried fruit, some injectables) - these can trigger asthma in sensitive people, but it’s not an immune reaction like a drug allergy
- Sulfur - the element. Found in eggs, garlic, and your own skin. Totally unrelated.
A 2020 survey found that 43% of primary care doctors mistakenly believed sulfites were unsafe for people with sulfa allergies. That’s misinformation with real consequences. If you’re allergic to sulfonamide antibiotics, you can safely eat garlic, drink wine, or take Epsom salts.
The Future: Better Tools, Fewer Mistakes
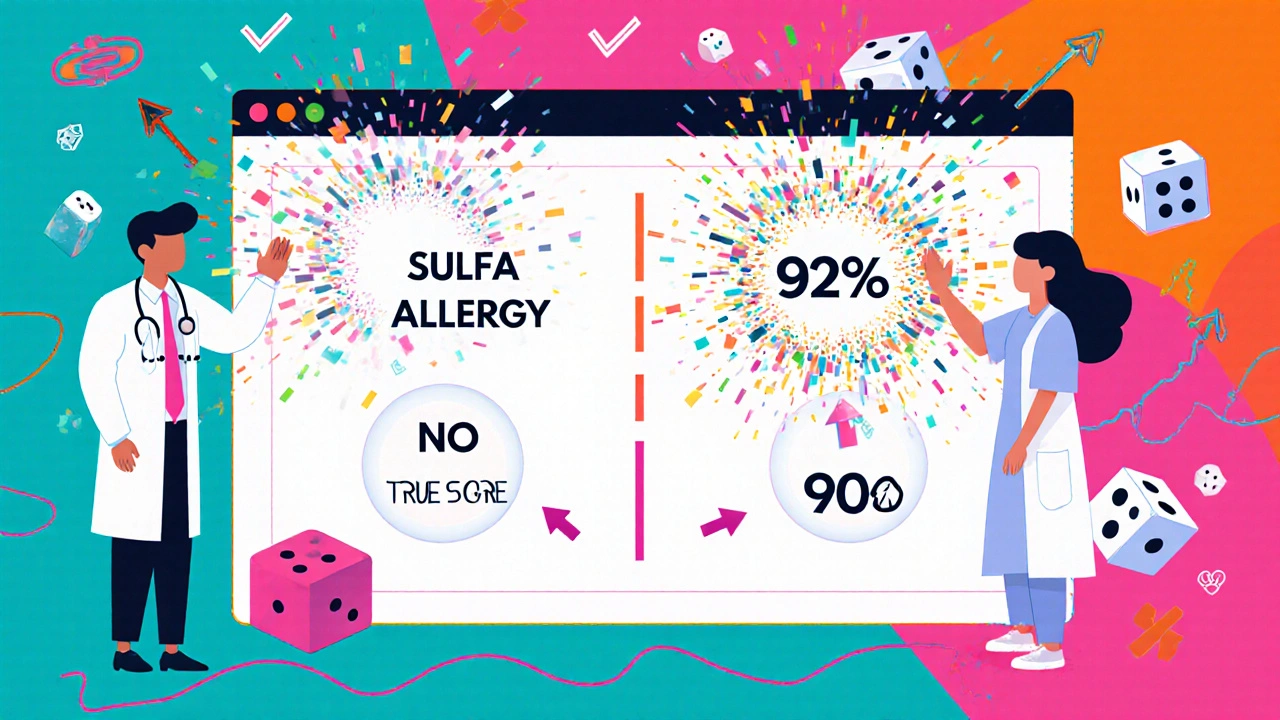
New tools are emerging. The SULF-RISK score, launched in 2022, helps doctors predict who’s likely to have a true allergy based on reaction type, timing, and symptoms. It’s 92% accurate. In 2023, clinical trials began testing a blood test that detects IgE antibodies specific to sulfamethoxazole-this could one day replace guesswork with a simple lab result.Hospitals are also updating their electronic health records. Systems like Epic now flag when a patient with a "sulfa allergy" label is prescribed hydrochlorothiazide or celecoxib-and suggest a review instead of blocking the prescription. In 2023, 68% of major U.S. hospitals had these alerts, up from just 22% in 2019.
But technology won’t fix everything. The biggest barrier is patient fear. A 2023 survey found that 68% of people with a "sulfa allergy" label believe they can’t take any medication with sulfur-even though sulfur isn’t involved. Education is key. You need to know the difference between chemistry and fear.
Can I take hydrochlorothiazide if I have a sulfa allergy?
Yes, you likely can. Hydrochlorothiazide is a nonantimicrobial sulfonamide and does not contain the chemical structure that triggers allergic reactions to antibiotic sulfonamides. Multiple studies show the risk of reaction is no higher than in people without any sulfa allergy history. If you’ve only had a mild rash from sulfamethoxazole, a supervised oral challenge can confirm tolerance.
Is celecoxib safe for people with sulfa allergies?
Yes. Celecoxib (Celebrex) is a nonantimicrobial sulfonamide. It lacks the N4-arylamine group that makes antibiotic sulfonamides allergenic. Large population studies show no increased risk of reaction in people with sulfonamide antibiotic allergies. In fact, the reaction rate is statistically the same as in people without any sulfa allergy history.
What’s the difference between sulfa allergy and sulfite allergy?
They’re completely different. A sulfa allergy is an immune reaction to certain antibiotics containing the sulfonamide group with an N4-arylamine. A sulfite allergy (more accurately, sulfite sensitivity) is a reaction to preservatives like sulfur dioxide, which can trigger asthma in some people. Sulfites are not related to sulfonamide drugs. Having one doesn’t mean you have the other.
Should I avoid all drugs with "sulf" in the name?
No. Only avoid sulfonamide antibiotics like sulfamethoxazole, sulfadiazine, and sulfasalazine if you’ve had a true allergic reaction. Other drugs like furosemide, acetazolamide, and metformin are safe. Even sulfate salts (like magnesium sulfate) and sulfites (in wine) are unrelated and safe for most people with sulfonamide antibiotic allergies.
Can a sulfa allergy be outgrown?
True IgE-mediated allergies don’t typically go away, but most people labeled with a sulfa allergy never had one to begin with. Many reactions from childhood were side effects, not allergies. Studies show that over 90% of people who undergo formal testing (like oral challenges) turn out to tolerate sulfonamide antibiotics or nonantimicrobial sulfonamides. If you were told you had a sulfa allergy years ago, it’s worth getting re-evaluated.
Next Steps: What to Do Today
If you’ve been told you have a sulfa allergy:- Check your medical records. What was the reaction? When did it happen? Was it an immediate rash, hives, or trouble breathing?
- Ask your doctor: "Was this a true allergy, or a side effect?"
- If you’re on blood pressure or diabetes meds and were denied them because of a sulfa label, ask about getting tested.
- If you’ve never had a severe reaction, consider a supervised challenge with hydrochlorothiazide or celecoxib-it’s safe and can free you from unnecessary restrictions.
- Update your allergy list. Replace "sulfa allergy" with the specific drug and reaction type, if possible.
Don’t let a label from 20 years ago limit your treatment options today. The science has changed. Your care should too.



November 15, 2025 AT 21:09 PM
So let me get this straight-just because some drug has 'sulf' in it doesn't mean I can't take it? My grandma’s been avoiding all meds with 'sulf' since 1998 because of a rash from Bactrim. Now you're telling me she could've been taking her blood pressure pills all along? This is wild.
November 17, 2025 AT 09:30 AM
Let’s be real-this is Big Pharma’s latest scam to sell you more expensive drugs. They don’t want you to know that sulfa antibiotics are cheap and effective, so they’ve been pushing this 'cross-reactivity myth' for decades. Why? Because celecoxib costs $300 a month and sulfamethoxazole is 50 cents. They rebranded the same chemical group to scare you into buying their overpriced alternatives. The FDA’s been in their pocket since 2003. Look up the 2017 whistleblower report-no one talks about it because you’ll get banned from Reddit for saying it.
November 18, 2025 AT 04:48 AM
It is imperative to emphasize that the distinction between antimicrobial and nonantimicrobial sulfonamides is not merely semantic-it is biochemically and immunologically substantiated. The structural determinants of allergic response, particularly the N4-arylamine moiety, are absent in nonantibiotic sulfonamides such as hydrochlorothiazide and celecoxib. Consequently, the clinical recommendation to avoid these agents based on a history of sulfonamide antibiotic allergy lacks scientific validity. Patients should be referred to allergists for formal de-labeling, particularly when alternative therapies are suboptimal or contraindicated. This is not speculation-it is evidence-based medicine.
November 19, 2025 AT 19:04 PM
It’s fascinating how we assign meaning to chemical structures as if they carry moral weight. The sulfonamide group is just atoms arranged in space-our fear of it is a cultural artifact, a story we tell ourselves to feel safe. But safety isn’t in the molecule. It’s in the context. The label 'allergy' becomes a ritual. We don’t question it because to question it would mean admitting we’ve been wrong for years. And that’s harder than any rash.
November 21, 2025 AT 12:41 PM
Okay but let’s not oversimplify. The 1.3% reaction rate sounds low, but when you’re the one getting SJS, that’s 100%. Also, 'nonantimicrobial sulfonamide' is just corporate jargon for 'we changed the formula so we can patent it.' I’ve seen patients react to HCTZ after a Bactrim rash-yes, rare, but it happens. Don’t tell me to just 'get tested' when my PCP won’t even order the test because 'it’s not worth it.' This isn’t just science-it’s access to care.
November 22, 2025 AT 18:07 PM
huh. so i can take lasix? cool. didn't know that. my doctor just said 'no sulfa' and that was it. guess i'll ask next time.
November 23, 2025 AT 21:16 PM
Man, this hits deep. I had a reaction to Bactrim in college-hives, swelling, panic attack. I’ve avoided anything with 'sulf' ever since. Then last year, my cardiologist said, 'You’re not allergic to HCTZ.' I laughed. I cried. I took the pill. No reaction. I’ve been on it for a year now. But here’s the thing-it wasn’t the science that freed me. It was the courage of one doctor who didn’t take my label at face value. We’ve turned medical labels into identity. 'I’m the sulfa-allergic person.' But you’re not. You’re someone who had a bad reaction once. That’s not who you are. It’s just a chapter. And you get to rewrite it.
November 25, 2025 AT 19:42 PM
Look, I used to think 'sulfa allergy' meant I couldn’t eat shrimp because 'sulfur' was in both. I thought that for 15 years. Then I read this and realized I’d been scared of a ghost. The real tragedy isn’t the drug-I mean, sure, it’s expensive and confusing-but it’s how we’ve let fear replace curiosity. We don’t ask questions. We just say 'no' because someone told us to. We’re not taught to think about chemistry. We’re taught to obey labels. And now we’re paying for it-in money, in health, in trust. If we could just pause for a second and ask 'why?' instead of 'what’s the warning label say?'-we’d be a lot healthier. Not just physically. Mentally too.
November 26, 2025 AT 20:37 PM
Oh wow. So my 20-year-old 'sulfa allergy' label is just a glitch in the system? And now I can finally take my blood pressure med without being treated like a walking biohazard? Thank you. Seriously. I’ve been on lisinopril for years because my doctor was too scared to try HCTZ. Now I’m gonna print this out, walk into my PCP’s office, and say, 'I’m not allergic to anything except bad medicine.' And I’m gonna do it with a smirk.
November 28, 2025 AT 10:29 AM
This is a very important message for global health. In many countries, doctors do not have access to allergy testing, and patients are denied life-saving medications due to outdated labels. I have seen patients in rural India avoid diuretics for heart failure simply because they were told 'no sulfa.' This information must be translated into local languages and shared with community health workers. A simple poster saying 'Not all sulfa drugs are the same' could save lives. Thank you for writing this clearly. Let us not let fear replace knowledge.