When you walk into a pharmacy to pick up a prescription, you might be handed a pill that looks nothing like the one you’ve taken before. It’s a different color, shape, or size - and it costs a fraction of what you paid last time. That’s a generic drug. And for most people, it’s just as effective as the brand-name version. But not everyone feels the same way. Some swear by their original medication. Others have had bad experiences switching. So what’s really going on? Are generics just cheap copies, or are they truly the same?
What Makes a Generic Drug a Generic Drug?
A generic drug isn’t a copycat. It’s a legal, FDA-approved duplicate of a brand-name drug. To get approved, it must contain the exact same active ingredient, in the same strength, and delivered the same way - whether it’s a pill, injection, or inhaler. The FDA doesn’t allow any wiggle room here. If the active ingredient is 10 mg of lisinopril, the generic must be 10 mg of lisinopril. No more, no less.
The big difference? The inactive stuff. Fillers, dyes, binders, and coatings can vary. That’s why a generic version of metformin might be white and oval, while the brand-name version is blue and round. These differences don’t affect how the drug works. But they can matter if you’re allergic to a specific dye or have trouble swallowing a large pill.
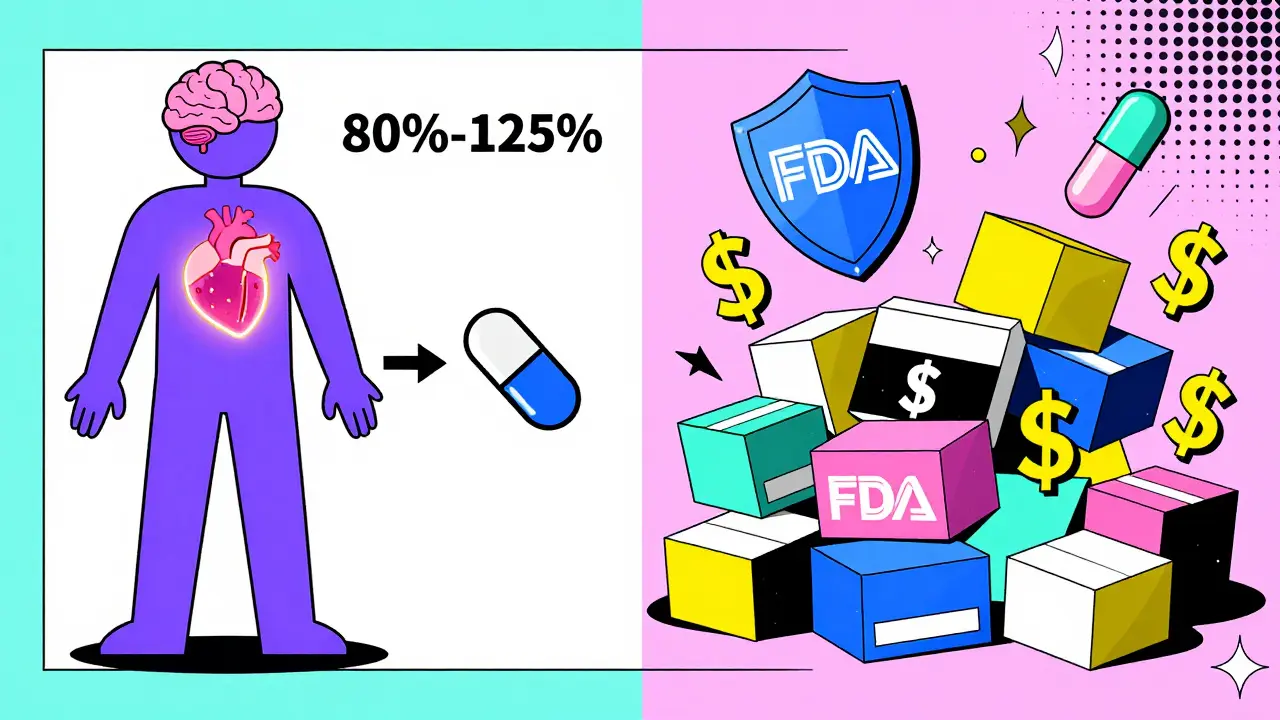
The FDA requires that generic manufacturers prove their product is bioequivalent to the brand-name drug. That means the generic must deliver the same amount of active ingredient into your bloodstream at the same speed. The acceptable range? Between 80% and 125% of the brand’s absorption rate. Most generics fall within 3.5% variation - barely more than random chance. A 2016 JAMA study looked at over 2,000 bioequivalence tests and found no meaningful difference in outcomes for most patients.
Why Are Generics So Much Cheaper?
Brand-name drugs cost a fortune because their makers spend years and billions developing them. The FDA estimates it takes about $2.6 billion to bring a new drug to market - covering research, clinical trials, and regulatory hurdles. That’s why Lipitor, for example, cost $130 a month before its patent expired.
Generic makers don’t have to repeat all that. They just need to prove their version works the same. That cuts development costs by 90%. No marketing campaigns. No TV ads. No patent protection. So when a brand-name drug’s patent runs out, multiple companies can start making the generic. Competition kicks in. Prices drop fast.
Take atorvastatin (Lipitor). After generics hit the market, the price fell from $130 to under $1 per month within five years. That’s not a fluke. From 2007 to 2016, generic drugs saved the U.S. healthcare system $1.67 trillion. Medicare alone saved $77 billion. For people on fixed incomes, that’s life-changing.
Are Generics Always Safe?
For most drugs, yes. The FDA holds generic manufacturing plants to the same standards as brand-name ones. Inspections, quality controls, and testing protocols are identical. A 2023 GAO report found that 18% of foreign generic facilities had FDA inspection issues - compared to 8% for U.S. plants. That’s a concern, but not a dealbreaker. Most generics, even those made overseas, meet safety standards.
But there’s a small group of drugs where even tiny changes matter. These are called narrow therapeutic index (NTI) drugs. They’re the kind where the difference between a therapeutic dose and a toxic one is razor-thin. Examples include warfarin (a blood thinner), levothyroxine (for thyroid disorders), and some epilepsy meds like phenytoin and carbamazepine.
For these, switching between different generic manufacturers can sometimes cause problems. A 2017 study from the University of Cincinnati Epilepsy Center found that switching between different generic versions of levetiracetam led to a 32% higher risk of seizure-related hospitalizations. Patients on Synthroid (levothyroxine) reported more side effects - like fatigue or heart palpitations - after switching to a different generic batch. That’s not because generics are unsafe. It’s because even small shifts in absorption can throw off delicate balances.
The American Academy of Neurology and the FDA both agree: for NTI drugs, consistency matters. If you’re stable on one generic brand, stick with it. Don’t let your pharmacist switch you without checking with your doctor.
What Do Real Patients Say?
Online forums are full of stories. On Reddit’s r/Pharmacy, one user saved $450 a month switching from brand-name Humira to its biosimilar. Another said their blood pressure stabilized after switching from brand to generic lisinopril. But there are also complaints. A Drugs.com analysis of 250,000 reviews found that 87% of users reported no difference with generics like metformin or atorvastatin. But 13% of people on thyroid meds said they felt worse after a switch.
Why? Often, it’s not the drug itself. It’s the change. Your body gets used to one formulation. Even if the new one is technically identical, your system might react to a slightly different filler or coating. That’s why some doctors recommend staying with the same generic manufacturer - especially for chronic conditions.
Medicare data shows that 68% of beneficiaries choose generics because of cost. Only 22% say their doctor recommended it. That’s a gap. Many patients don’t know they can ask to stay on one brand. Or that they can request a "dispense as written" note on their prescription.
When Should You Stick With Brand-Name?
You don’t need to avoid generics. But there are times when sticking with the brand makes sense:
- You’re on a narrow therapeutic index drug (warfarin, levothyroxine, epilepsy meds).
- You’ve had a bad reaction after switching generics.
- Your doctor specifically wrote "dispense as written" on the prescription.
- You’re taking a complex drug like an inhaler, topical cream, or injectable biologic - where generics (biosimilars) are still new and less predictable.
For most other drugs - antibiotics, statins, blood pressure pills, antidepressants - generics are just as safe and effective. And way cheaper.

How to Navigate the System
Here’s how to take control:
- Ask your pharmacist: "Is this a generic? Which manufacturer makes it?" Write it down.
- If you’re on an NTI drug, ask your doctor if you can request the same generic brand each time.
- Use GoodRx to compare prices. Sometimes the brand-name drug is cheaper than a particular generic - especially with coupons.
- Check the FDA’s Orange Book for therapeutic equivalence ratings. It lists which generics are rated "AB" (therapeutically equivalent) and which aren’t.
- If you notice new side effects after a switch, tell your doctor. Don’t assume it’s "all in your head."
Most pharmacies will automatically substitute generics unless told not to. That’s the law in 49 U.S. states. But you have the right to say no. Just ask.
The Big Picture
Generics aren’t a compromise. They’re a smart, safe, and widely used part of modern medicine. Nine out of ten prescriptions in the U.S. are filled with generics. That’s not because people are desperate. It’s because they work.
The savings aren’t just personal. They’re systemic. In 2022, generics made up 90% of prescriptions but only 26% of total drug spending. Brand-name drugs, which make up just 11% of prescriptions, cost 74% of the total. That imbalance is why healthcare systems push generics.
Future trends point to even more generics. Biosimilars - the next wave of generic biologics - are growing fast. Drugs like Humira, which cost over $20 billion a year, now have cheaper alternatives. The FDA is speeding up approvals and cracking down on quality control. By 2030, global generic use is expected to rise from 56% to 70% of all prescriptions.
Bottom line: For most people, generics are the clear choice. They’re not second-rate. They’re proven, tested, and trusted. But if you’re on a high-risk medication, don’t switch blindly. Know your drug. Know your options. And talk to your doctor before you make a change.
Are generic drugs as effective as brand-name drugs?
Yes, for the vast majority of medications. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. Studies show no meaningful difference in how well they work for most people. Over 90% of prescriptions in the U.S. are filled with generics because they’re proven to be just as effective.
Why do generic pills look different from brand-name pills?
U.S. trademark laws prevent generic manufacturers from making their pills look identical to brand-name drugs. So they change the color, shape, size, or markings. But the active ingredient is the same. These differences don’t affect how the drug works - they’re just for legal reasons. If you’re confused by the change, check the label or ask your pharmacist.
Can I switch between different generic brands?
For most drugs, yes. But for narrow therapeutic index (NTI) drugs like warfarin, levothyroxine, or certain seizure medications, switching between different generic manufacturers can cause problems. Even small differences in absorption can affect your health. If you’re on one of these, ask your doctor to specify "dispense as written" or stick with the same generic brand each time.
Are generic drugs made in the same facilities as brand-name drugs?
Sometimes. Many generic manufacturers use the same facilities as brand-name makers - or even produce the brand-name version under contract. The FDA inspects all facilities equally, whether they make generics or brands. But about 18% of foreign generic facilities had inspection issues in 2023, compared to 8% for U.S. ones. That doesn’t mean they’re unsafe, but it’s something to be aware of.
How much money can I save with generic drugs?
On average, generics cost 80% to 85% less than brand-name drugs. For example, the generic version of Lipitor dropped from $130 a month to under $1 after patent expiration. GoodRx reports an average savings of 82.5% across common medications. For chronic conditions, that can mean hundreds - or even thousands - of dollars saved each year.
Should I always choose the cheapest generic?
Not necessarily. While most generics are interchangeable, some people respond differently to different formulations - especially with NTI drugs. If you’ve had a good experience with one generic brand, stick with it. Use tools like GoodRx to compare prices, but don’t switch just because it’s cheaper. Talk to your doctor or pharmacist if you notice side effects after a switch.


January 29, 2026 AT 00:50 AM
Generics work fine unless you're on warfarin or levothyroxine then good luck