Steroid Hyperglycemia Insulin Adjustment Calculator
This calculator helps you determine appropriate insulin adjustments based on steroid dosage and your current insulin regimen. Use it as a guide in consultation with your healthcare provider.
Input Your Current Regimen
Why Steroids Make Blood Sugar Spike in People with Diabetes
If you’re taking steroids like prednisone or hydrocortisone and you have diabetes, you’ve probably noticed your blood sugar going haywire-even if you’ve been eating the same meals and taking the same meds. This isn’t just bad luck. It’s called steroid hyperglycemia, and it happens because steroids mess with how your body uses insulin.
Glucocorticoids, the type of steroids used for inflammation, autoimmune diseases, or after transplants, block insulin from doing its job. They make your liver dump more glucose into your blood, stop your muscles from absorbing sugar, and even reduce how much insulin your pancreas can produce. The result? Blood sugar spikes, especially after meals. Studies show over 50% of people on high-dose steroids develop noticeable hyperglycemia, and nearly half stay above 140 mg/dL all day long.
How Steroids Change Your Body’s Glucose Control
Steroids don’t just raise blood sugar randomly. They follow a pattern. When you take a dose in the morning, your blood sugar peaks 4 to 8 hours later. That’s why breakfast and lunch are the hardest meals to manage-not dinner. This is the opposite of typical type 2 diabetes, where fasting glucose is the main concern.
The science behind it is straightforward: steroids interfere with insulin signaling. They shut down key proteins like GLUT4 that move glucose into cells. They also boost glucagon, a hormone that tells your liver to release even more sugar. If you’re already insulin resistant, steroids make it worse. In fact, patients on hydrocortisone equivalents of 100 mg daily are over five times more likely to need insulin than those not on steroids.
And it’s not just about the dose. Longer treatment, older age, being overweight, or having had prediabetes before increases your risk. Even certain other medications make it worse. Tacrolimus, used after organ transplants, cuts insulin production by 35-45%. Low magnesium levels? Each 0.1 mg/dL drop raises your chance of high blood sugar by 10-15%.
What Happens When You Start Steroids? Insulin Needs Go Up
If you already take insulin, your dose will likely need to increase-sometimes dramatically. Experts like Dr. Guillermo Umpierrez recommend a 30-50% rise in total daily insulin when starting moderate to high-dose steroids (20 mg prednisone or more). For newly diagnosed steroid-induced diabetes, a basal-bolus insulin plan is far better than just using sliding scale insulin.
Here’s how to break it down:
- Basal insulin: Increase by 20-30%. This covers your background sugar production, which steroids ramp up all day.
- Mealtime insulin: Increase by 50-100%, especially for breakfast and lunch. That’s when steroid levels peak.
For example, someone on 40 units of basal insulin and 30 units of mealtime insulin daily might need to jump to 50-55 units basal and 50-60 units mealtime. It’s not guesswork-it’s based on steroid pharmacokinetics.
Patients on once-daily morning steroids rarely need extra insulin at dinner. But if you’re on multiple daily doses, like hydrocortisone every 8 hours, you’ll need to adjust insulin at every meal. The timing matters as much as the amount.
Monitoring Blood Sugar During Steroid Therapy
Checking your blood sugar once a day won’t cut it. You need to know what’s happening after meals. The Endocrine Society recommends at least four daily checks: fasting, and 2 hours after breakfast, lunch, and dinner. If your numbers are climbing, go to six or eight checks a day.
Many people rely on fasting glucose, but that’s misleading. Steroid hyperglycemia is mostly post-meal. One study found fasting glucose misses 15-20% of cases. That’s why using a continuous glucose monitor (CGM) is a game-changer. A 2021 Dexcom case series showed CGM users adjusted insulin doses 37% more accurately than those using fingersticks.
Look for patterns. If your lunchtime sugar is always above 180 mg/dL but dinner is fine, you’re probably under-dosed for breakfast. If your bedtime sugar drops too low, you might be over-dosed for dinner. Track your steroid doses alongside your glucose readings. Most apps let you tag events-do it.
When Steroids Are Stopped: The Hidden Danger of Hypoglycemia
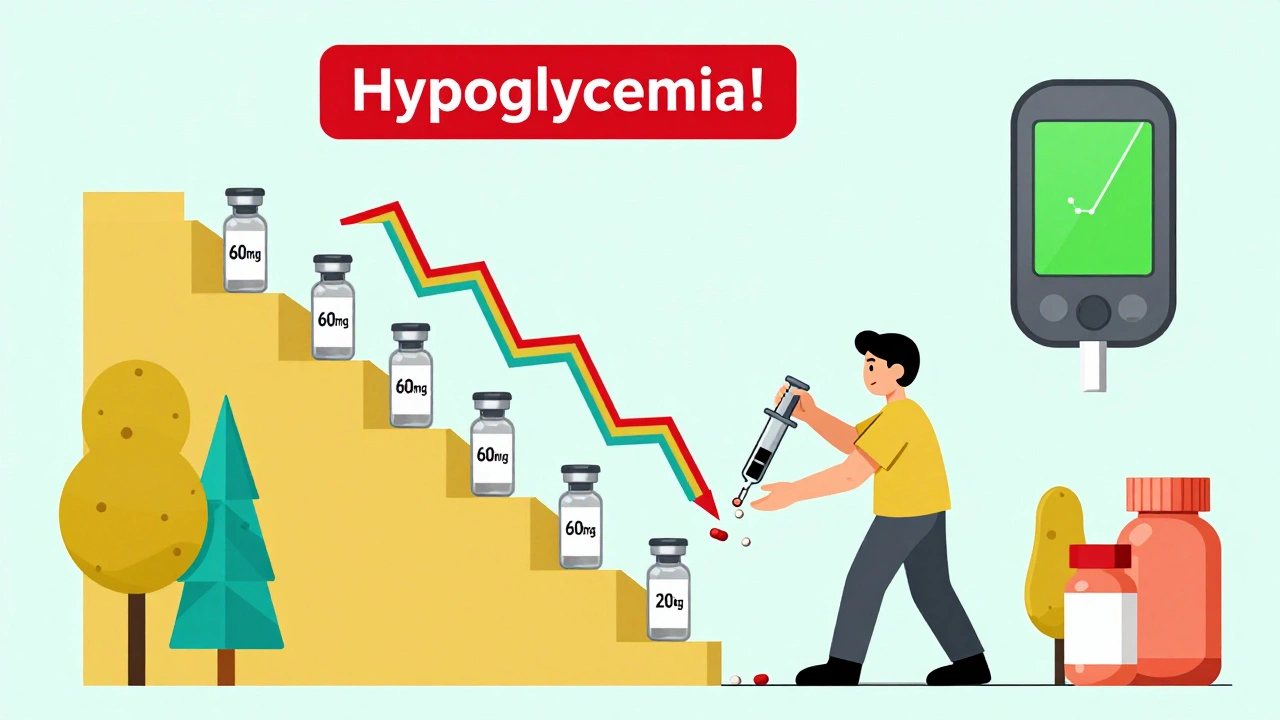
The biggest mistake? Not lowering insulin when the steroid dose goes down.
Steroid hyperglycemia doesn’t disappear overnight. But as the steroid effect fades, your insulin needs drop fast. If you keep your high dose, your blood sugar can crash. A Johns Hopkins study found 18% of hospital readmissions within 30 days of stopping steroids were due to hypoglycemia from unchanged insulin regimens.
Dr. Robert Rushakoff from UCSF warns that over-aggressive insulin use during steroid therapy leads to dangerous lows during tapering. In one study, 22% of patients had hypoglycemia because their insulin wasn’t reduced.
Here’s the rule: For every 10 mg reduction in prednisone equivalent, cut your total daily insulin by 10-20%. If you’re on 60 mg prednisone and drop to 50 mg, reduce insulin by 10-12%. Go down to 40 mg? Cut another 10-20%. Don’t wait for your doctor to tell you. Monitor closely and adjust proactively.
Some patients taper steroids over weeks. That’s when daily glucose logs become essential. If you’re using an insulin pump or smart insulin pen, program in temporary basal rates or correction factors as the steroid dose drops.
What About Oral Diabetes Medications?
Most oral meds aren’t enough for steroid-induced hyperglycemia. Metformin helps a little with insulin resistance, but it won’t control the big spikes. Sulfonylureas can cause dangerous lows, especially as steroids taper. SGLT2 inhibitors? Risky-steroids increase dehydration risk, and these drugs raise the chance of diabetic ketoacidosis.
GLP-1 agonists like semaglutide might help with weight and insulin sensitivity, but they’re slow-acting and not ideal for acute steroid spikes. DPP-4 inhibitors? Too mild.
Bottom line: Insulin is the gold standard during steroid therapy. Oral meds are fine for baseline control, but they’re not enough when steroids hit. Most endocrinologists will switch patients to insulin while on steroids and reassess later.
Special Cases: Kids, Transplant Patients, and Chronic Steroid Users
Pediatric patients on high-dose steroids (like for asthma or kidney disease) often need 25-40% more total insulin, with even bigger jumps in mealtime doses. Their bodies respond faster, and their insulin needs change daily. Parents need clear, written plans.
Transplant patients are a double challenge. They’re on steroids plus tacrolimus or cyclosporine-both of which crush insulin production. These patients often need 2-3 times their pre-transplant insulin dose. Their glucose levels can swing wildly. CGM and insulin pumps are often essential.
For people on long-term steroids-say, for lupus or COPD-this becomes a chronic issue. The American Diabetes Association now recommends that anyone on steroids for more than 7 days should be screened for hyperglycemia. Some hospitals are using AI tools that predict insulin needs based on steroid dose, BMI, and HbA1c. One 2023 trial cut hyperglycemia episodes by 41% using this approach.
What Works in Real Life: Patient Stories and Pro Tips
Reddit’s r/diabetes community has over 140 posts from people who’ve been through this. The most common theme? “I didn’t know my insulin needed to change.”
- One man on 40 mg prednisone for polymyalgia needed 80% more insulin. He started checking glucose 2 hours after every meal and dropped his lunchtime dose by 30% when he cut prednisone to 20 mg.
- A woman on dexamethasone for brain swelling had stable sugars until she switched to prednisone. Her glucose spiked overnight because prednisone peaks faster. She switched from long-acting insulin to a mix of basal and rapid-acting, and it stabilized.
- Another patient used her CGM to see that her sugar stayed high even after eating salad. She realized steroids were pushing her liver to make sugar-so she increased her basal insulin, not her carbs.
Pro tips:
- Keep a log: steroid dose, time taken, glucose readings, insulin given.
- Use mealtime insulin analogs (like lispro or aspart)-they work faster and match steroid peaks better.
- Don’t skip meals to avoid high sugar. That just makes it worse later.
- Ask your doctor for a steroid-specific insulin adjustment plan before you start treatment.
What’s Changing in 2025: New Tools and Guidelines
Hospitals are catching on. The Joint Commission now requires specific hyperglycemia protocols for steroid patients. Over 90% of U.S. hospitals with 200+ beds have them. Tools like EndoTool and Glytec’s eGlucose system use algorithms to recommend insulin doses based on steroid type and dose. Hospitals using these tools saw 27% fewer hyperglycemia events.
Future tech is even smarter. Mayo Clinic is testing systems that auto-adjust insulin pumps when steroids are administered. Real-time glucose data feeds into the pump, and it changes basal rates automatically. Early results show 38% better time-in-range.
By 2027, experts predict 75% of U.S. hospitals will have formal steroid hyperglycemia protocols. But outside hospitals, many primary care doctors still don’t know how to adjust insulin. That’s where patients need to be their own advocates. Know your numbers. Know your steroid. Know your insulin.

December 2, 2025 AT 14:01 PM
Steroid hyperglycemia is just insulin resistance on steroids lol. Basal up 20-30 bolus 50-100. Done. No magic just math.
December 3, 2025 AT 13:02 PM
bro i was on 60mg prednisone for my eczema and my sugars went to 400+ like wtf?? i thought i was eating bad but nooo it was the steroids. i started using my cgms and it was a game changer. 🤯
December 5, 2025 AT 03:27 AM
This is so important. I’ve been managing T2D for 8 years and never realized how dramatically steroids affect postprandial spikes. The fact that breakfast and lunch are the hardest makes total sense now. I’ve started logging my steroid doses with my glucose readings - it’s like having a second brain. 🙌
December 6, 2025 AT 01:17 AM
It's fascinating how the medical community still treats steroid-induced hyperglycemia as an afterthought. The reality is that endocrinologists are often the only ones who understand this, while primary care physicians remain dangerously complacent. This isn't just about insulin adjustments - it's about systemic neglect of metabolic physiology in the face of pharmaceutical intervention. And yet, patients are left to self-educate via Reddit threads. Pathetic.
December 7, 2025 AT 06:18 AM
You people are overcomplicating this. If your blood sugar spikes on steroids, you're just lazy. Stop eating carbs. Problem solved. I’ve seen people on 100mg prednisone and still eating bagels like it’s a buffet. You want to live in denial? Fine. But don’t blame the medicine.
December 8, 2025 AT 06:10 AM
There’s something deeply human about how our bodies react to external chemical forces - steroids don’t just alter glucose metabolism, they expose the fragility of our metabolic equilibrium. We think we control our health through diet and medication, but when a pill like prednisone enters the system, it reminds us we’re not in charge. The real challenge isn’t adjusting insulin - it’s accepting that sometimes, our bodies need to be held by science, not just guided by will.
December 10, 2025 AT 03:48 AM
i was on steroids after kidney transplant and my insulin needs tripled. i didnt know what to do so i just kept adding units until i passed out. then i learned. cgms saved my life. also tacrolimus is the real villain here
December 11, 2025 AT 06:16 AM
Let me guess - you’re one of those people who thinks insulin is the ‘gold standard’ because some 2023 paper said so. Meanwhile, in the real world, people are dying from insulin overdoses during tapering because doctors are too lazy to educate. The real ‘gold standard’ is patient autonomy. Learn your numbers. Don’t rely on algorithms or EndoTool. Your pancreas might be broken, but your brain isn’t.
December 12, 2025 AT 04:39 AM
Oh wow. Another 2000-word essay on how to adjust insulin. Did you also write a 10-page PDF on how to breathe while standing up? 🙄 I mean, I get it. You’re a hero for reading a study. But let’s be real - most people just want to know if they should take more insulin or if they’re going to die. Keep your jargon. I’ll stick with my CGM and common sense.
December 12, 2025 AT 05:34 AM
Steroid dose up insulin up. Steroid down insulin down. Simple. No need for apps or algorithms. Just watch your numbers.
December 13, 2025 AT 23:44 PM
The pathophysiology of glucocorticoid-induced insulin resistance involves downregulation of IRS-1 and GLUT4 translocation, compounded by hepatic gluconeogenesis upregulation via PEPCK and G6Pase. Clinical management requires dynamic titration of basal-bolus regimens. Failure to recognize this cascade leads to iatrogenic hypoglycemia during tapering - a documented mortality risk.
December 15, 2025 AT 09:42 AM
So let me get this straight - you’re telling me I have to change my insulin because some doctor gave me a pill to stop my inflammation? Like, why didn’t they just give me the pill that doesn’t turn me into a diabetic? I’m tired of being a lab rat.
December 16, 2025 AT 21:02 PM
I’ve been on prednisone for 18 months for lupus. My husband says I’m a different person. I’m not just high on sugar - I’m high on rage. I cry when I see my glucose numbers. I hate this. No one talks about the emotional toll. Just ‘increase basal by 20%’. Like I’m a machine.
December 17, 2025 AT 23:16 PM
You got this. It’s overwhelming at first, but tracking your numbers and adjusting slowly makes all the difference. You’re not alone - so many of us have been there. One day at a time 💪❤️
December 18, 2025 AT 20:17 PM
The real issue here isn’t just insulin dosing - it’s the lack of standardized protocols across healthcare systems. In a hospital setting, where steroid use is predictable and monitored, these adjustments are routine. But in outpatient primary care? It’s a lottery. Patients are expected to self-manage complex pharmacokinetic interactions with zero guidance. This isn’t patient empowerment - it’s negligence dressed up as education. We need mandatory diabetes education for prescribers of glucocorticoids, not just for patients. The system is failing us.
December 18, 2025 AT 23:16 PM
The notion that insulin is the 'gold standard' for steroid-induced hyperglycemia is a reductive medical dogma that ignores the broader epistemological framework of metabolic adaptation. The body does not merely 'respond' to exogenous glucocorticoids - it reconfigures its entire endocrine architecture in real time. To treat this as a linear pharmacological problem - increase basal, increase bolus - is to mistake the symptom for the system. The real question is not how much insulin to administer, but whether the medical paradigm itself, rooted in reductionist biochemistry, is capable of comprehending the emergent complexity of human physiology under pharmacological duress. We are not adjusting doses - we are negotiating with a living system that resists quantification.